Category: Parkinson's Disease: Neuroimaging
Objective: To evaluate whether patients with multiple sclerosis who develop parkinsonism have significant differences in regional lesion burden compared to multiple sclerosis patients who do not develop parkinsonism.
Background: While multiple sclerosis (MS) and Parkinsonism/Parkinson’s disease (PoPD) represent independent disease processes, there have been multiple case reports of co-occurrence and nationwide cohort studies suggesting higher incidence rates and risk of PD in the MS population. There have been no studies beyond case reports comparing imaging characteristics of patients with and without this co-diagnosis to clarify the potential pathophysiologic basis of the increased risk of PD.
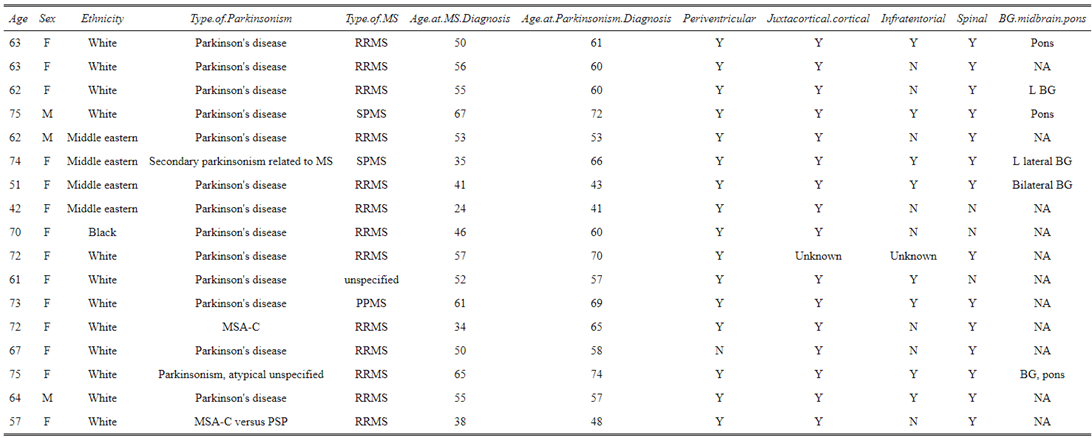
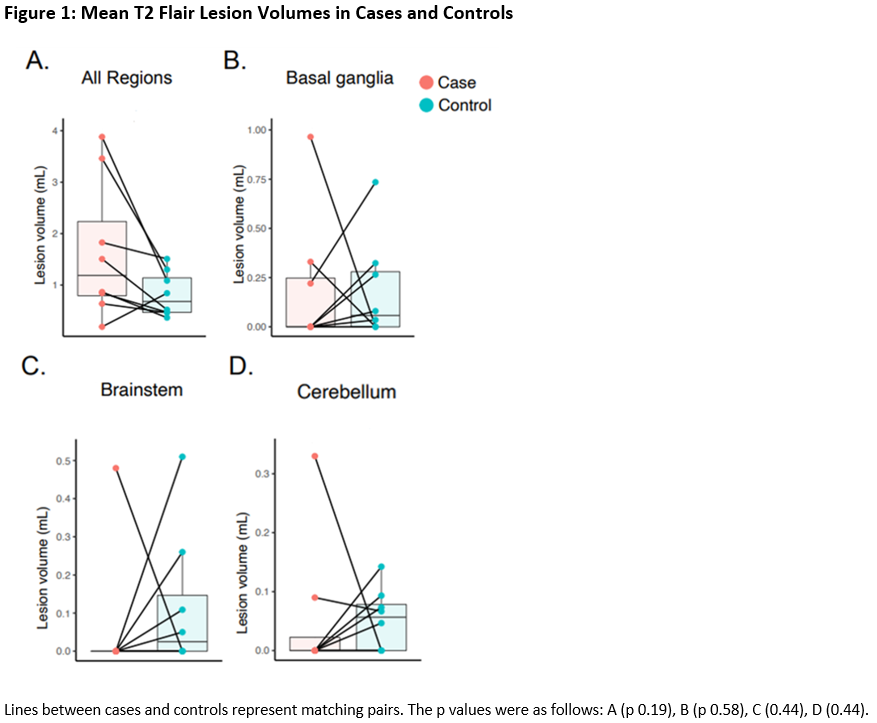
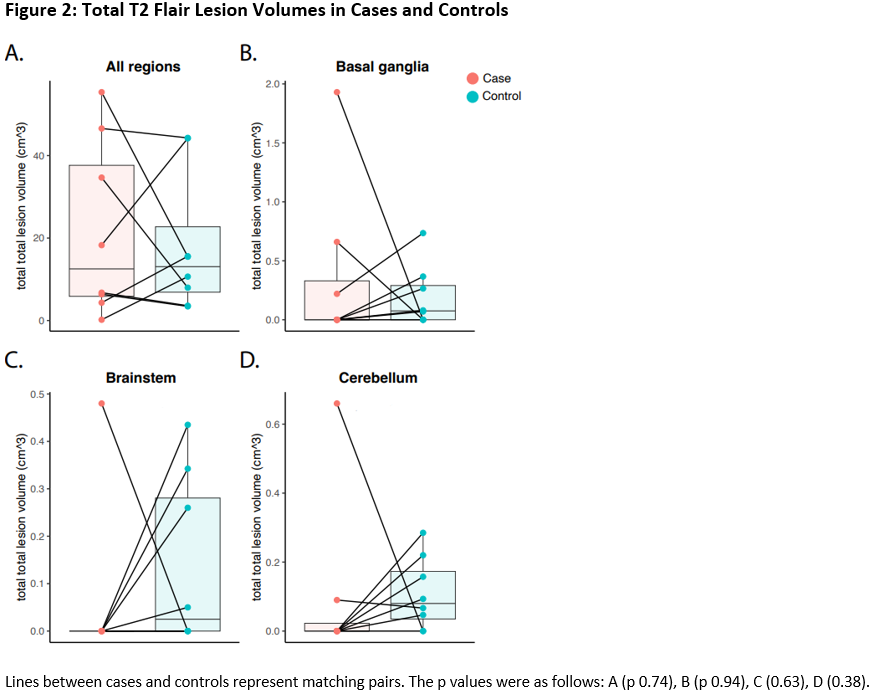
Method: We reviewed medical records from 2012-2022 within a single health care system for patients with multiple sclerosis and parkinsonism. An ICD code search resulted in 104 patients; on manual chart review 17 patients met final inclusion criteria. Ten patients had available MRI brain images for which lesion quantification was possible. Eight patients could be matched 1:3 to a control MS only cohort by sex, age at MS diagnosis, and MRI images near the age of PoPD diagnosis. T2 FLAIR lesions were identified and outlined with livewire mode segmentation to calculate volumes. Volume and location (basal ganglia, brainstem, cerebellum) were recorded for each lesion.
Results: Among 17 cases, the age of onset of MS ranged from 24-67 with a mean of 49 and median of 52, which was an older cohort compared to the general MS population where the age of diagnosis typically ranges from 20-49. The age of PoPD diagnosis ranged from 41-74 (mean 59). For the eight cases in which MRI images and controls were available, Wilcoxon matched pairs signed rank test showed no statistically significant difference in lesion burden globally or in specific regions (basal ganglia, brainstem, cerebellum) between cases and controls. There was a potential trend of increased global lesion burden in the co-diagnosis group that did not reach statistical significance (mean lesion volume p=0.19, total lesion volume p=0.74).
Conclusion: Our preliminary data did not find a statistically significant difference in white matter lesion burden globally or regionally in the comparative MRI brain image analysis between eight patients with a dual diagnosis of MS and PoPD and a matched cohort of MS patients who did not develop PoPD.
References: 1. Schultheiss T, Reichmann H, Ziemssen T. Rapidly progressive course of very late onset multiple sclerosis presenting with Parkinsonism: case report. Mult Scler. 2011;17(2):245-249.
2. Ozturk V, Idiman E, Sengun IS, Yuksel Z. Multiple sclerosis and parkinsonism: a case report. Funct Neurol. 2002;17(3):145-147.
3. Shaygannejad V, Shirmardi M, Dehghani L, Maghzi H. Co-occurrence of multiple sclerosis and Parkinson disease. Adv Biomed Res. 2016;5:75.
4. Vieregge P, Klostermann W, Brückmann H. Parkinsonism in multiple sclerosis. Mov Disord. 1992;7(4):380-382.
5. Valkovic P, Krastev G, Mako M, Leitner P, Gasser T. A unique case of coincidence of early onset Parkinson’s disease and multiple sclerosis. Mov Disord. 2007;22(15):2278-2281.
6. Tranchant C, Bhatia KP, Marsden CD. Movement disorders in multiple sclerosis. Mov Disord. 1995;10(4):418-423.
7. Saidha S, Mok TH, Butler M, Fanning N, Harrington H. Multiple sclerosis exceptionally presenting as parkinsonism responds to intravenous methylprednisolone. J Clin Neurosci. 2010;17(5):654-655.
8. Barun B, Brinar VV, Zadro I, Lusić I, Radović D, Habek M. Parkinsonism and multiple sclerosis–is there association? Clin Neurol Neurosurg. 2008;110(9):958-961.
9. Damásio J, Ramos C, Valdemar L, da Silva AM, Magalhães M. A coincidental case of young-onset Parkinson disease and multiple sclerosis. Neurologist. 2011;17(5):286-288.
10. Mao CC, Gancher ST, Herndon RM. Movement disorders in multiple sclerosis. Mov Disord. 1988;3(2):109-116.
11. Folgar S, Gatto EM, Raina G, Micheli F. Parkinsonism as a manifestation of multiple sclerosis. Mov Disord. 2003;18(1):108-110.
12. Federlein J, Postert T, Allgeier A, Hoffmann V, Pöhlau D, Przuntek H. Remitting parkinsonism as a symptom of multiple sclerosis and the associated magnetic resonance imaging findings. Mov Disord. 1997;12(6):1090-1091.
13. Kreisler A, Stankoff B, Ribeiro MJ, Agid Y, Lubetzki C, Fontaine B. Unexpected aggravation of Parkinson’s disease by a mesencephalic multiple sclerosis lesion. J Neurol. 2004;251(12):1526-1527.
14. Nielsen NM, Pasternak B, Stenager E, Koch-Henriksen N, Frisch M. Multiple sclerosis and risk of Parkinson’s disease: a Danish nationwide cohort study. European Journal of Neurology. 2014;21(1):107-111.
15. Thormann A, Magyari M, Koch-Henriksen N, Laursen B, Soelberg-Sorensen P. Parkinson’s Disease in Multiple Sclerosis – A Population-Based, Nationwide Study in Denmark (P2.186). Neurology. 2016;86(16 Supplement).
16. Kwon S, Jung SY, Han KD, Jung JH, Yeo Y, Cho EB, Ahn JH, Shin DW, Min JH. Risk of Parkinson’s disease in multiple sclerosis and neuromyelitis optica spectrum disorder: a nationwide cohort study in South Korea. J Neurol Neurosurg Psychiatry. 2022 Jul 28:jnnp-2022-329389. doi: 10.1136/jnnp-2022-329389. Epub ahead of print. PMID: 35902226.
17. Sarin S, Wang A, Elkasaby M, Abboud H. Parkinsonism in multiple sclerosis patients: A prospective observational study. Mult Scler Relat Disord. 2022 Jun;62:103796. doi: 10.1016/j.msard.2022.103796. Epub 2022 Apr 10. PMID: 35428029.
18. Buscarinu MC, Reniè R, Morena E, Romano C, Bellucci G, Marrone A, Bigi R, Salvetti M, Ristori G. Late-Onset MS: Disease Course and Safety-Efficacy of DMTS. Front Neurol. 2022 Mar 10;13:829331. doi: 10.3389/fneur.2022.829331. PMID: 35356454; PMCID: PMC8960027.
19. Pagano G, Ferrara N, Brooks DJ, Pavese N. Age at onset and Parkinson disease phenotype. Neurology. 2016 Apr 12;86(15):1400-1407. doi: 10.1212/WNL.0000000000002461. Epub 2016 Feb 10. PMID: 26865518; PMCID: PMC4831034.
20. Filippi M, Preziosa P, Banwell BL, Barkhof F, Ciccarelli O, De Stefano N, Geurts JJG, Paul F, Reich DS, Toosy AT, Traboulsee A, Wattjes MP, Yousry TA, Gass A, Lubetzki C, Weinshenker BG, Rocca MA. Assessment of lesions on magnetic resonance imaging in multiple sclerosis: practical guidelines. Brain. 2019 Jul 1;142(7):1858-1875. doi: 10.1093/brain/awz144. PMID: 31209474; PMCID: PMC6598631.
To cite this abstract in AMA style:
Y. Shi, S. Gadani, K. Mills. White Matter Lesion Characteristics of Patients with Multiple Sclerosis and Parkinsonism [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/white-matter-lesion-characteristics-of-patients-with-multiple-sclerosis-and-parkinsonism/. Accessed April 26, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/white-matter-lesion-characteristics-of-patients-with-multiple-sclerosis-and-parkinsonism/