Session Information
Date: Monday, October 8, 2018
Session Title: Parkinson's Disease: Non-Motor Symptoms
Session Time: 1:15pm-2:45pm
Location: Hall 3FG
Objective: To determine the neuropsychiatric and non-motor correlates of reduced physical activity in PD.
Background: The motor symptoms of PD interfere with patients’ ability to perform significant physical activity and exercise. However, it is less clear whether resultant underactivity is linked to non-motor symptoms.
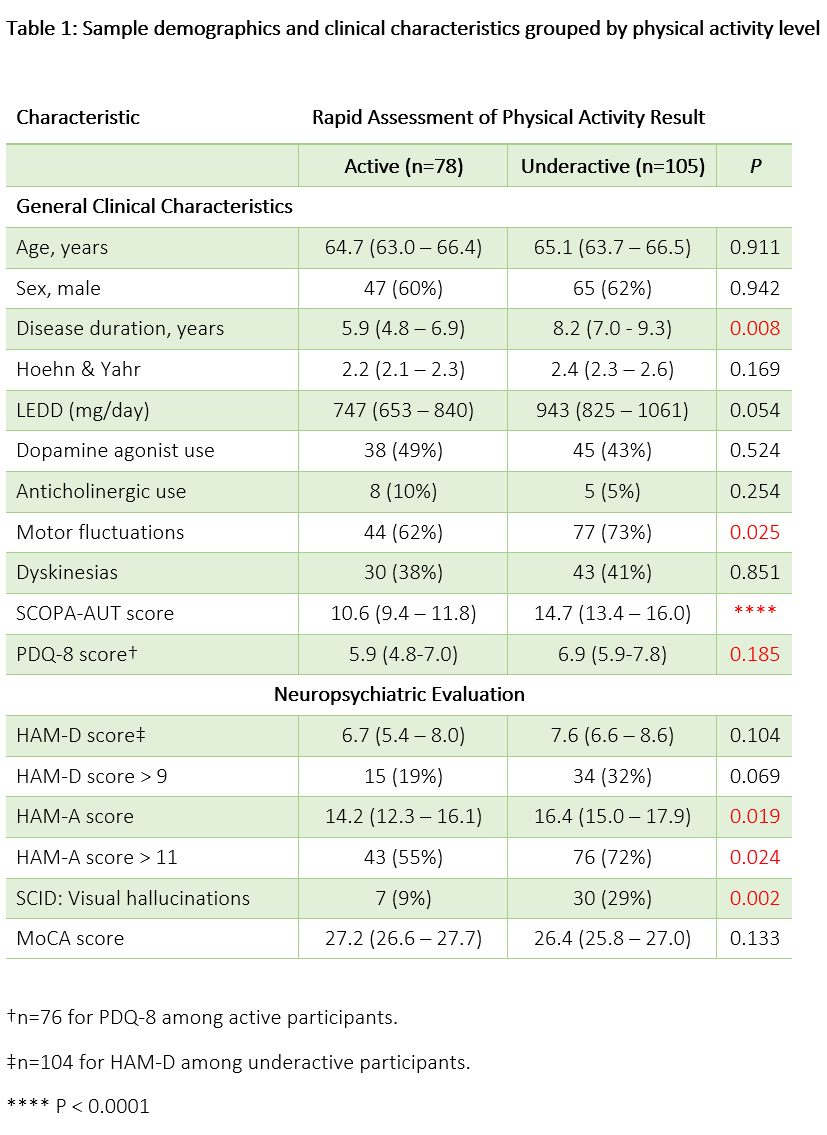
Methods: Data for 183 PD participants were drawn from an ongoing study of PD anxiety. The Rapid Assessment of Physical Activity (RAPA) scale groups older adults as “active” if they do either (1) over 30 minutes of moderate exercise at least 5 days/week, or (2) over 20 minutes of vigorous exercise at least 3 days/week. Visual hallucinations (VH) were assessed by structured clinical interview in accordance with DSM-IV-TR criteria. Autonomic dysfunction was reported using the Scales for Outcomes in Parkinson’s Disease-Autonomic questionnaire (SCOPA-AUT). Stepwise regression was used to reduce a saturated list of clinical and demographic variables for binomial regression using physical underactivity as the outcome.
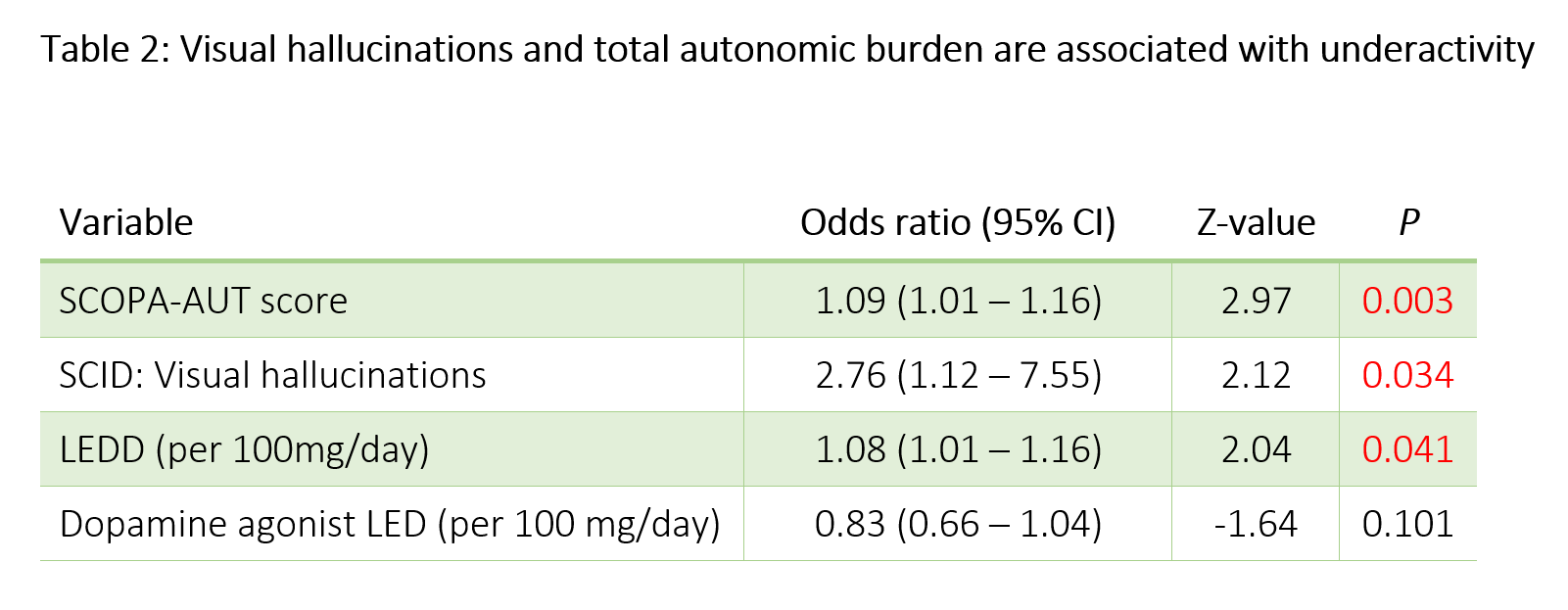
Results: RAPA survey results indicated that 105 (57.4%) were underactive (i.e. did not meet criteria for “active”) [table1]. Underactivity was significantly associated with higher total SCOPA-AUT score (U=5479, P<0.0001), longer disease duration (U=5028, P=0.008), and the presence of motor fluctuations (χ2=5.0, P = 0.025), but not higher Hoehn & Yahr stage. VH (χ2=9.5, P = 0.002) and clinically significant anxiety (HAM-A > 11) were also associated with underactivity (χ2=5.1, P=0.024). Multivariable analysis with logistic regression [table2] demonstrated that total SCOPA-AUT score (Z = 3.0, P = 0.003), VH (Z = 2.1, P = 0.034), and total non-DA agonist levodopa equivalent dose (LED) (Z = 2.0, P = 0.041) were significantly associated with underactivity. The model adjusted for dopamine agonist LED, which did not significantly associate with physical activity; additionally, no significant interaction was noted between VH and total LED or agonist LED.
Conclusions: Autonomic burden and VH were more strongly associated with underactivity than disease duration or Hoehn & Yahr stage in our participants. Exercise-based trials and activity-monitoring will be required to determine whether these symptoms impede physical activity or if underactivity serves as a risk factor for these non-motor complications.
To cite this abstract in AMA style:
J. Hinkle, K. Perepezko, N. Fischer, Z. Mari, L. Marsh, G. Pontone. Visual hallucinations and autonomic burden are inversely associated with physical activity in PD [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/visual-hallucinations-and-autonomic-burden-are-inversely-associated-with-physical-activity-in-pd/. Accessed December 29, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/visual-hallucinations-and-autonomic-burden-are-inversely-associated-with-physical-activity-in-pd/