Category: Surgical Therapy: Parkinson's Disease
Objective: To investigate whether video-based evaluations of motor control and changes of predefined stimulation parameters via patient programmer can improve motor status in Parkinson’s disease patients with deep brain stimulation (DBS).
Background: While studies have shown, that telemedical care can be delivered to patients with movement disorders [1-3], there are only few reports on those with DBS [4,5].
Method: We included ten patients who received two weeks of home-based video treatment. Patients recorded daily videos of a modified version of the Unified Parkinson’s Disease Rating Scale Part III [6]. After regular evaluations of these videos by two physicians at the DBS-center, patients received phone calls and were instructed to change amplitudes and alternate predefined stimulation programs by using the handheld programmer.
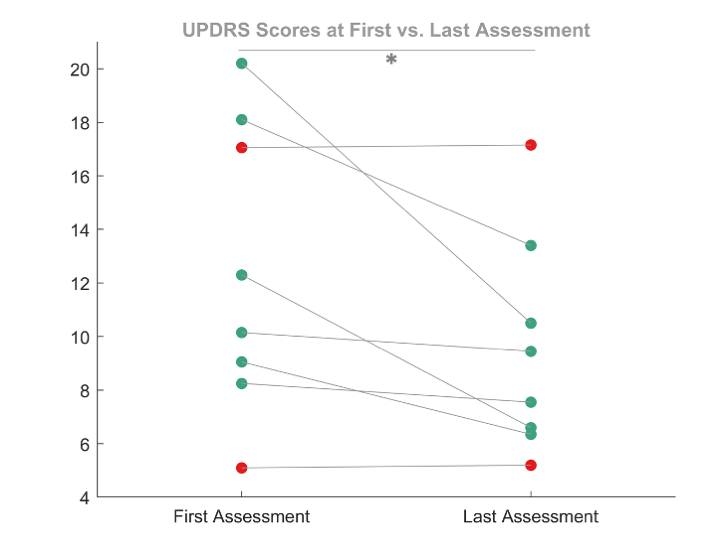
Results: Eight patients completed the study. Baseline motor status as measured by a modified version of the Unified Parkinson’s Disease Rating Scale Part III [6] significantly improved (p = 0.0313) compared to follow up after completion of the video treatment [figure 1].
Conclusion: We conclude that telemedical optimization by means of video assessments is feasible for this patient population but cannot replace in-person contacts in all cases.
References: [1] Hanson RE, Truesdell M, Stebbins GT, et al. Telemedicine vs Office Visits in a Movement Disorders Clinic: Comparative Satisfaction of Physicians and Patients. Movement Disorders Clinical Practice 2019;6:65–9. doi:10.1002/mdc3.12703
[2] Dorsey ER, Okun MS, Bloem BR. Care, Convenience, Comfort, Confidentiality, and Contagion: The 5 C’s that Will Shape the Future of Telemedicine. J Parkinsons Dis 2020;10:893–7. doi:10.3233/JPD-202109
[3] Dorsey ER, Bloem BR, Okun MS. A New Day: The Role of Telemedicine in Reshaping Care for Persons With Movement Disorders. Mov Disord 2020;35:1897–902. doi:10.1002/mds.28296
[4] Jitkritsadakul O, Rajalingam R, Toenjes C, et al. Tele-health for patients with deep brain stimulation: The experience of the Ontario Telemedicine Network. Movement Disorders 2018;33:491–2. doi:10.1002/mds.27230
[5] Zhang C, Zhu K, Lin Z, et al. Utility of Deep Brain Stimulation Telemedicine for Patients With Movement Disorders During the COVID-19 Outbreak in China. Neuromodulation: Technology at the Neural Interface 2021;24:337–42. doi:10.1111/ner.13274
[6] Fahn S, Elton R, Committee UD. Unified Parkinson’s Disease Rating Scale In: Fahn S, Marsden CD, Calne D, Goldstein M, eds. Recent Developments in Parkinson’s Disease Florham Park, NJ: Macmillan Healthcare Information 1987;2:153-163.
To cite this abstract in AMA style:
C. Schedlich-Teufer, H. Jergas, J. Steffen, J. Strelow, H. Dafsari, V. Visser-Vandewalle, M. Barbe, J. Wirths. Video-guided Optimization of Stimulation Settings in Patients with Parkinson’s Disease and Deep Brain Stimulation [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/video-guided-optimization-of-stimulation-settings-in-patients-with-parkinsons-disease-and-deep-brain-stimulation/. Accessed March 3, 2026.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/video-guided-optimization-of-stimulation-settings-in-patients-with-parkinsons-disease-and-deep-brain-stimulation/