Session Information
Date: Thursday, June 8, 2017
Session Title: Other
Session Time: 1:15pm-2:45pm
Location: Exhibit Hall C
Objective: 1) To calculate diagnostic accuracy of the Movement Disorder Society (MDS) prodromal criteria to predict conversion to Parkinson’s disease (PD) or dementia with Lewy bodies (DLB); 2) to evaluate the association between prodromal PD likelihood ratios and the time to conversion and 3) to investigate the independency of prodromal markers.
Background: Recently, the MDS introduced the prodromal criteria for PD. Accuracy of the MDS criteria for prodromal PD needs to be validated, particularly in different cohorts in which the markers are combined.
Methods: This prospective cohort study was performed on 121 individuals with REM sleep behaviour disorder (RBD) who were followed annually for an average of 3.6 years. Using data from a comprehensive panel of prodromal markers, likelihood ratio (LR) and post-test probability of the criteria were calculated at baseline and during each follow-up visit.
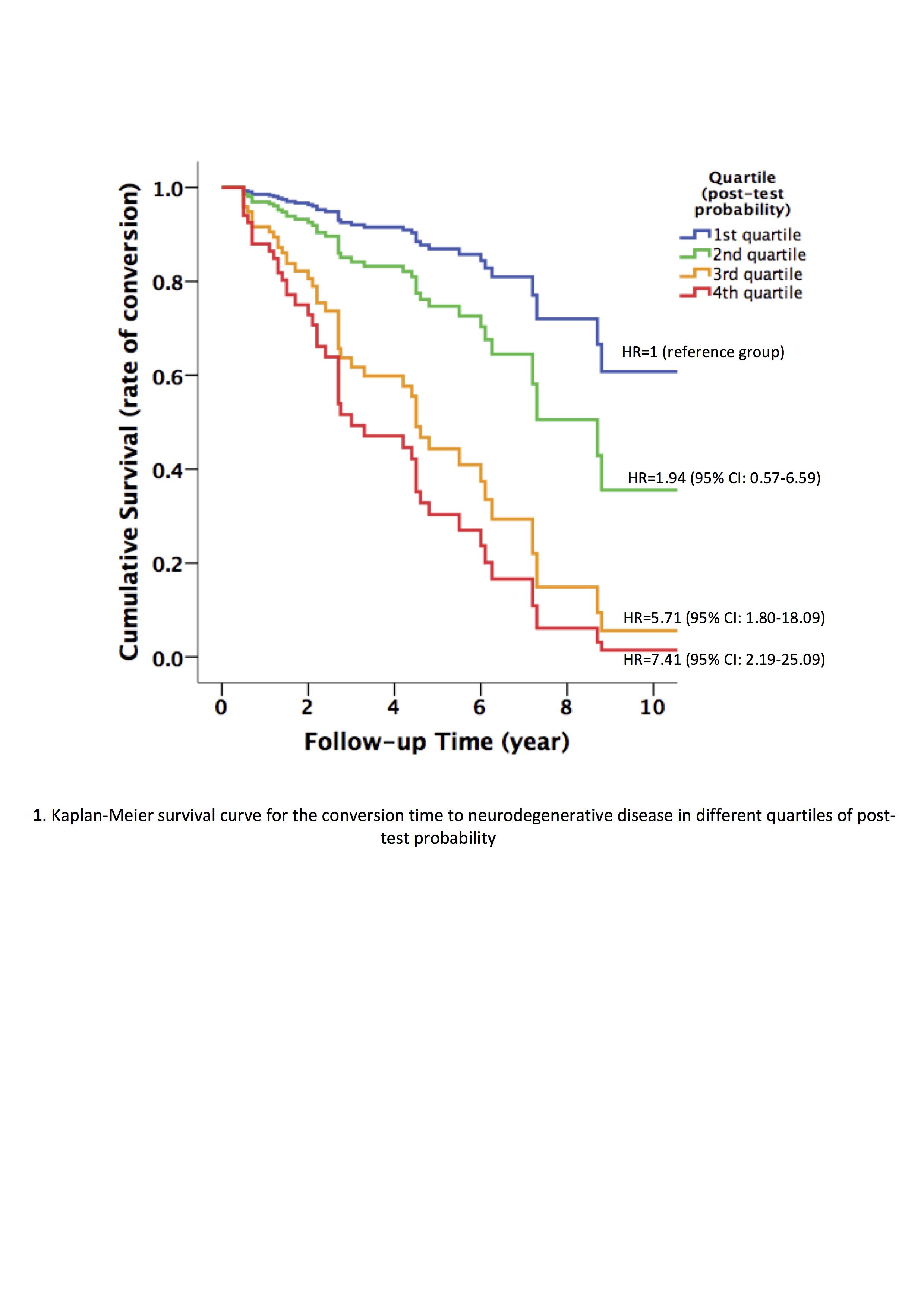
Results: Forty-eight (39.7%) individuals with RBD converted to PD/DLB. The MDS prodromal criteria had 81.3% sensitivity and 67.9% specificity for conversion to PD/DLB at 4-years follow-up. One year before conversion, sensitivity was 100%. The criteria predicted DLB with even higher accuracy than PD without dementia at onset. Those who met the threshold of prodromal criteria at baseline had significantly more rapid conversion into a neurodegenerative state (4.8 vs. 9.1 years, p<0.001). Furthermore, there was a stepwise increase in conversion rates according to the quartiles of the baseline post-test probability of prodromal PD calculated by from the MDS criteria (Figure 1). Pairwise combinations of different prodromal markers showed that markers were independent of each other except for a significant interaction between hyposmia and quantitative motor testing.
Conclusions: The MDS prodromal criteria are a promising tool for predicting incidence of PD/DLB and conversion time in an RBD cohort. In RBD, they have high sensitivity and negative predictive value (NPV). Prodromal markers influence the overall LR independently, allowing them to be reliably multiplied. Increasing the number of markers, further longitudinal assessment and testing of different thresholds in different target populations will continue to improve the criteria.
References: Berg D, Postuma RB, Adler CH, et al. MDS research criteria for prodromal Parkinson’s disease. Mov Disord 2015; 30(12): 1600-11.
To cite this abstract in AMA style:
S.-M. Fereshtehnejad, J. Montplaisir, A. Pelletier, J.-F. Gagnon, D. Berg, R. Postuma. Validation of the MDS Research Criteria for Prodromal Parkinson’s Disease: longitudinal assessment in a REM sleep behavior disorder (RBD) cohort [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/validation-of-the-mds-research-criteria-for-prodromal-parkinsons-disease-longitudinal-assessment-in-a-rem-sleep-behavior-disorder-rbd-cohort/. Accessed December 18, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/validation-of-the-mds-research-criteria-for-prodromal-parkinsons-disease-longitudinal-assessment-in-a-rem-sleep-behavior-disorder-rbd-cohort/