Session Information
Date: Wednesday, September 25, 2019
Session Title: Epidemiology
Session Time: 1:15pm-2:45pm
Location: Les Muses, Level 3
Objective: Verification of the previously reported association between chronic use of β2-adrenoreceptor (β2AR) agonist and antagonist with reduced and increased risk of Parkinson’s disease (PD), respectively.
Background: Based on the Norwegian national health registries, use of β2-adrenoreceptor agonists was associated with a reduced risk of Parkinson’s disease (PD), while β2-adrenoreceptor antagonist use was associated with an increased PD risk. PD risk modifying properties of such widely used drugs would have profound public health implications.
Method: We obtained odds ratio associating time of b2AR agonist and antagonist use with PD risk in nationwide Danish health registries.
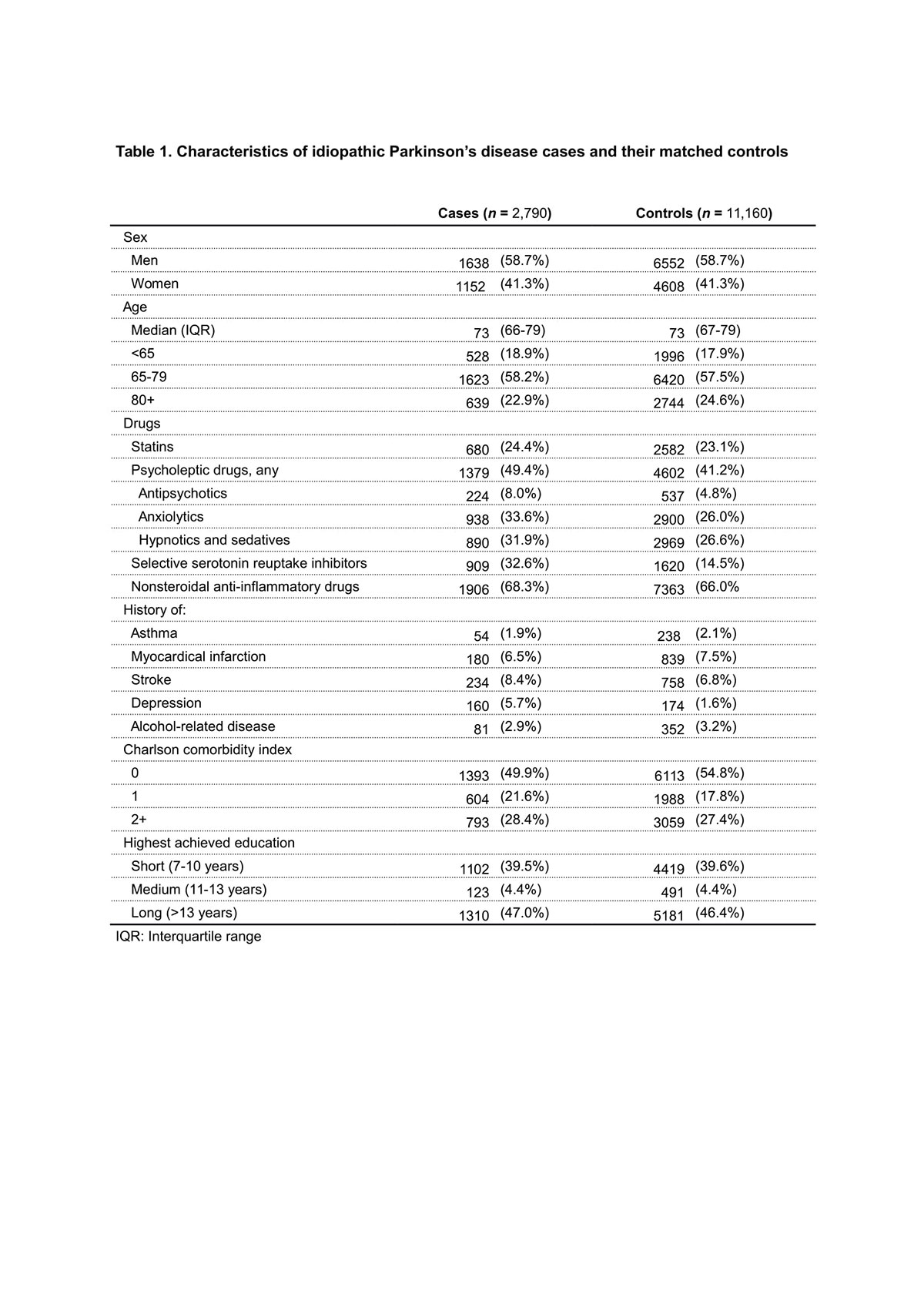
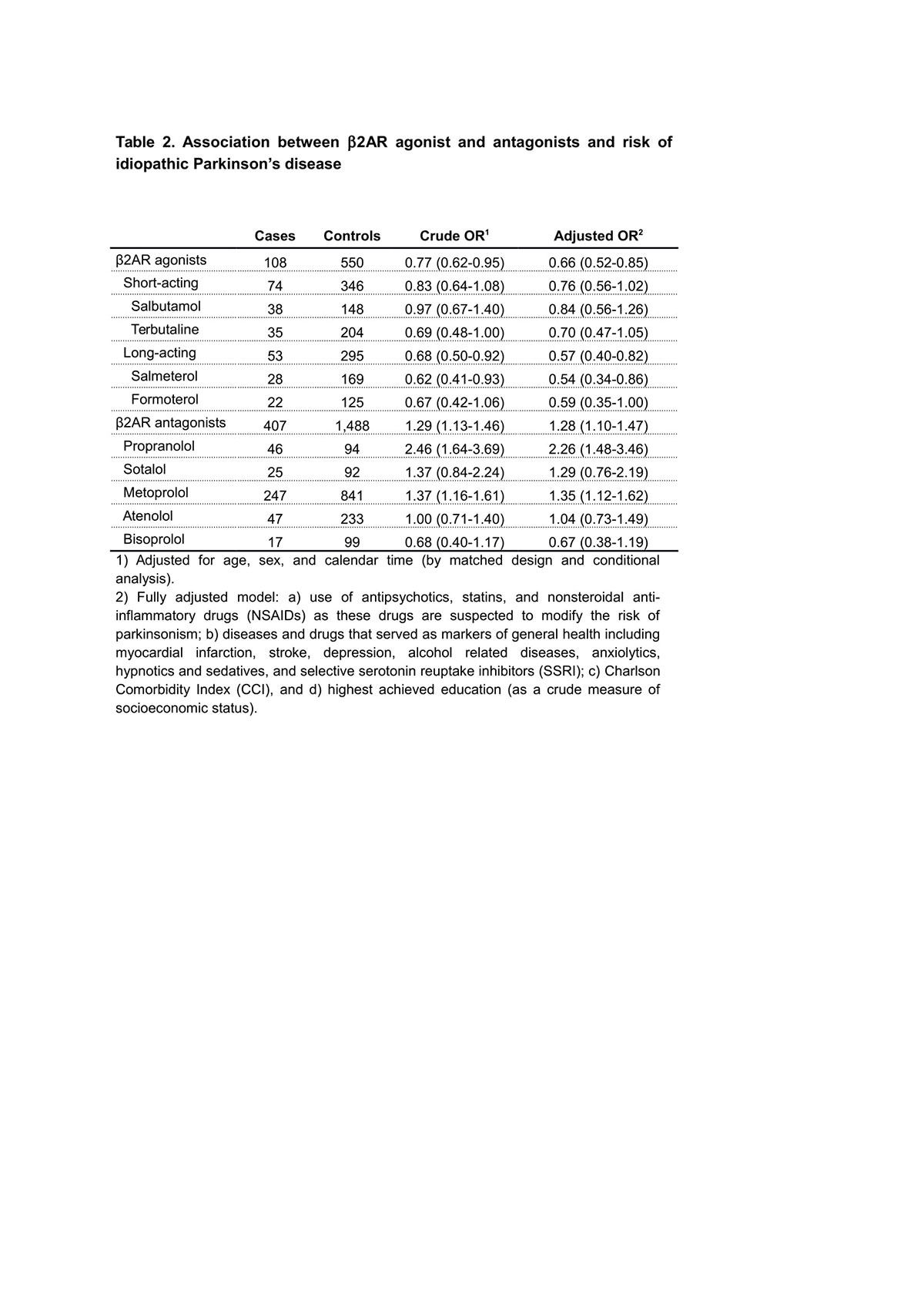
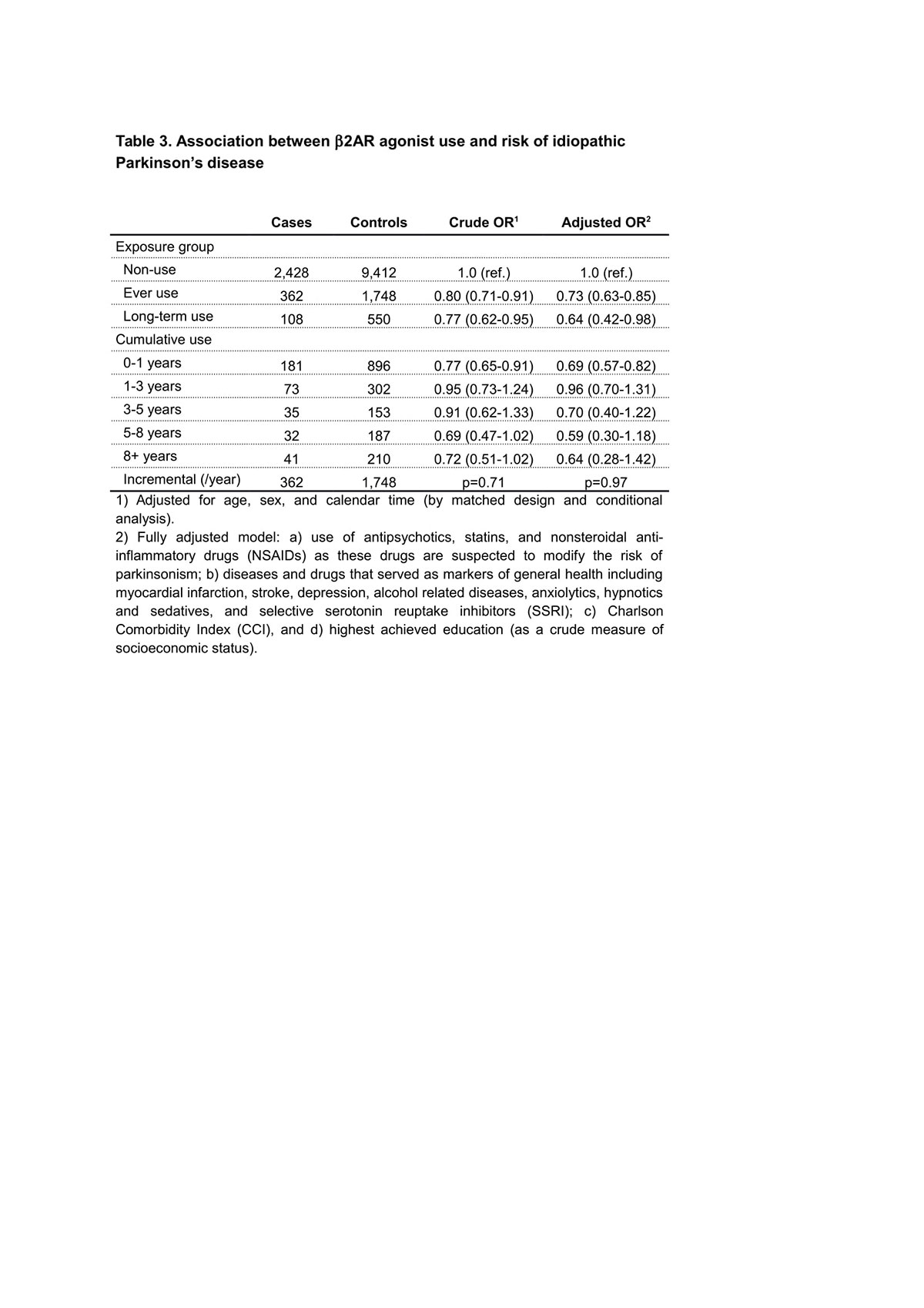
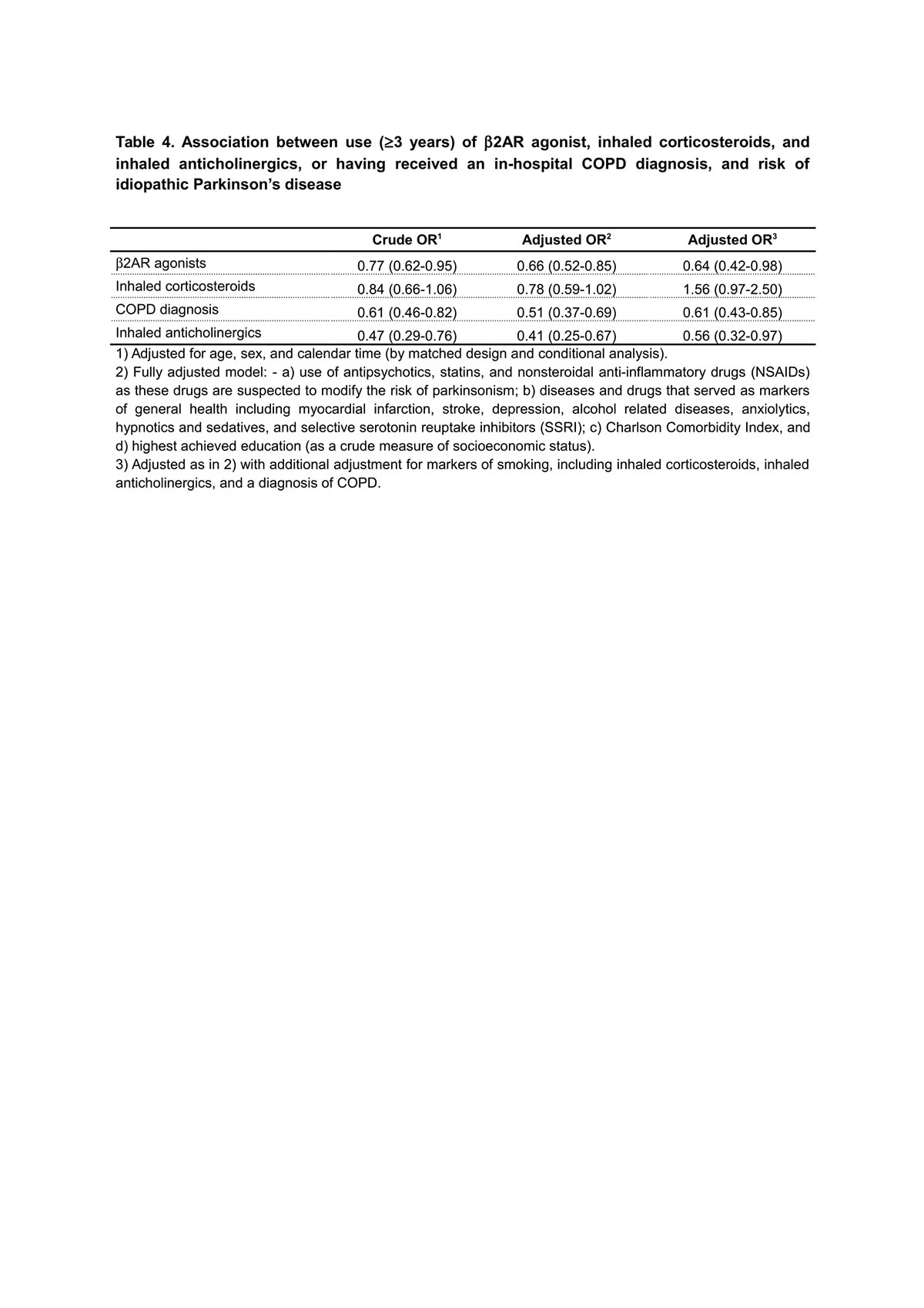
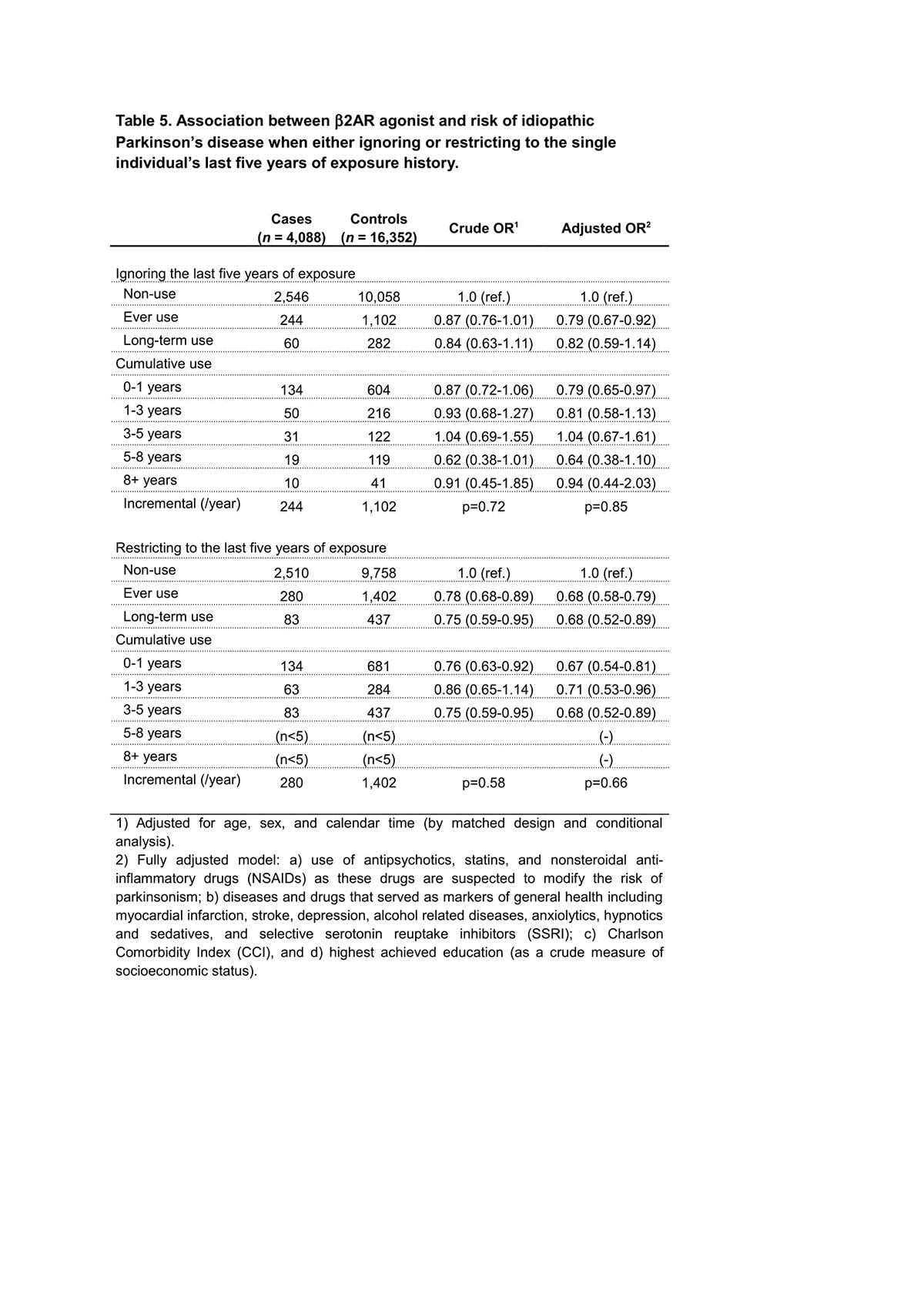
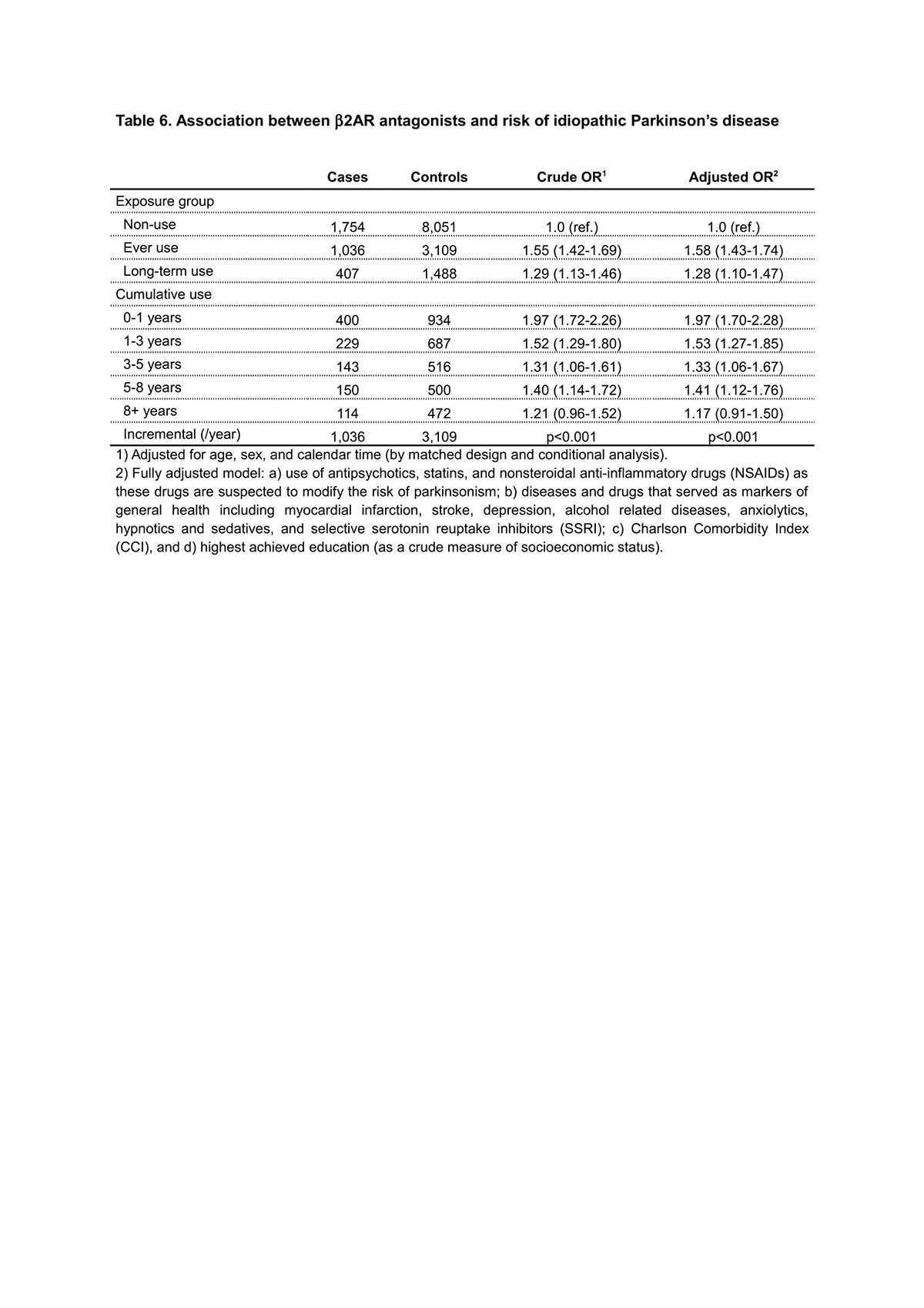
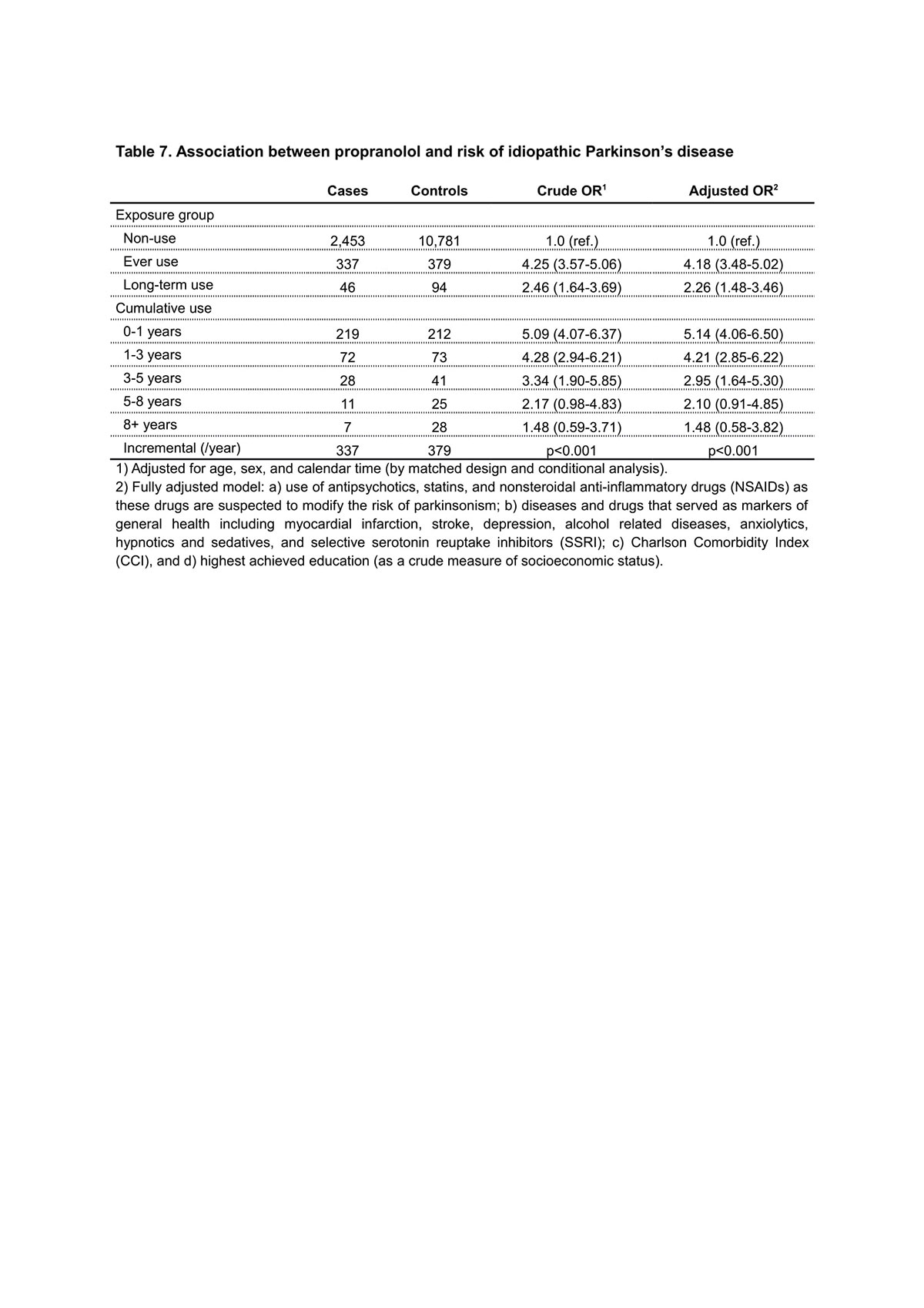
Results: 2,790 PD patients and 11,160 controls were included. Long-term β2AR agonist use was associated with reduced PD risk (OR 0.57; 95% CI 0.40-0.82) also in this cohort. Unexpectedly, short-term β2AR agonist use was equally associated (OR 0.64; 95% CI 0.42-0.98). Since β2AR agonists are mostly prescribed for chronic obstructive pulmonary disease (COPD), often caused by chronic nicotine abuse, we analyzed other markers of smoking. Diagnosis of COPD (OR 0.51; 95% CI 0.37-0.69), use of inhaled corticosteroids (OR 0.78; 95% CI 0.59-1.02) or inhaled anticholinergics (OR0.41; 95% CI 0.25-0.67) were also inversely associated with PD. Increased PD risk was not found for all β2AR antagonists, but only for propranolol and metoprolol. Associations were markedly stronger for short-term than long-term use.
Conclusion: We confirmed β2AR agonist use to be associated with reduced PD risk and β2AR antagonist use with increased PD risk. However, our data indicate the association of β2AR agonists to be indirectly mediated by smoking, which is repeatedly associated with reduced risk of PD. The association of β2AR antagonists indicates reverse causation, with PD symptoms triggering their prescription, rather than β2AR antagonists causing PD. Thus, current epidemiological data does not support a causal link between b2AR agonists and antagonists and PD risk.
References: 1. Gronich N, Abernethy DR, Auriel E, Lavi I, Rennert G, Saliba W. beta2-adrenoceptor agonists and antagonists and risk of Parkinson’s disease. Mov Disord 2018;33:1465-1471. 2. Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol 2015;7:449-490. 3. Pottegard A, Schmidt SAJ, Wallach-Kildemoes H, Sorensen HT, Hallas J, Schmidt M. Data Resource Profile: The Danish National Prescription Registry. Int J Epidemiol 2017;46:798-798f. 4. Pedersen CB. The Danish Civil Registration System. Scand J Public Health 2011;39:22-25. 5. Sortso C, Thygesen LC, Bronnum-Hansen H. Database on Danish population-based registers for public health and welfare research. Scand J Public Health 2011;39:17-19. 6. Kildemoes HW, Sorensen HT, Hallas J. The Danish National Prescription Registry. Scand J Public Health 2011;39:38-41. 7. Rothman KJ, Greenland S, Lash TL. Modern epidemiology, 3rd ed. ed. Philadelphia, Pa. ; London: Lippincott Williams & Wilkins, 2008. 8. Stovring H, Pottegard A, Hallas J. Determining prescription durations based on the parametric waiting time distribution. Pharmacoepidemiol Drug Saf 2016;25:1451-1459. 9. Stovring H, Pottegard A, Hallas J. Refining estimates of prescription durations by using observed covariates in pharmacoepidemiological databases: an application of the reverse waiting time distribution. Pharmacoepidemiol Drug Saf 2017;26:900-908. 10. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-383. 11. Rabe KF, Watz H. Chronic obstructive pulmonary disease. Lancet 2017;389:1931-1940. 12. Ritz B, Ascherio A, Checkoway H, et al. Pooled analysis of tobacco use and risk of Parkinson disease. Arch Neurol 2007;64:990-997. 13. Ascherio A, Schwarzschild MA. The epidemiology of Parkinson’s disease: risk factors and prevention. Lancet Neurol 2016;15:1257-1272. 14. Decramer M, Janssens W, Miravitlles M. Chronic obstructive pulmonary disease. Lancet 2012;379:1341-1351. 15. Rascol O. “Disease-modification” trials in Parkinson disease: target populations, endpoints and study design. Neurology 2009;72:S51-58. 16. Csizmadi I, Collet J-P, Boivin J-F. Bias and Confounding in Pharmacoepidemiology. Pharmacoepidemiology: John Wiley & Sons, Ltd, 2007: 791-809. 17. Postuma RB, Berg D, Stern M, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 2015;30:1591-1601. 18. Deuschl G, Raethjen J, Hellriegel H, Elble R. Treatment of patients with essential tremor. Lancet Neurol 2011;10:148-161. 19. Mittal S, Bjornevik K, Im DS, et al. beta2-Adrenoreceptor is a regulator of the alpha-synuclein gene driving risk of Parkinson’s disease. Science 2017;357:891-898. 20. WHO. The Selection and Use of Essential Medicines: WHO Expert Committee, World Health Organization, 2017.
To cite this abstract in AMA style:
F. Hopfner, M. Wod, G. Höglinger, M. Blaabjerg, T. Roesler, G. Kuhlenbäumer, K. Christensen, G. Deuschl, A. Pottegård. Use of ß2-adrenoreceptor agonist and antagonist drugs and risk of Parkinson’s disease [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/use-of-s2-adrenoreceptor-agonist-and-antagonist-drugs-and-risk-of-parkinsons-disease/. Accessed December 29, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/use-of-s2-adrenoreceptor-agonist-and-antagonist-drugs-and-risk-of-parkinsons-disease/