Session Information
Date: Wednesday, September 25, 2019
Session Title: Non-Motor Symptoms
Session Time: 1:15pm-2:45pm
Location: Agora 3 West, Level 3
Objective: This study aimed to determine the prevalence, associated factors of SH/NH and to identify relationships between blood pressure (BP) and sleep position in PD patients.
Background: Autonomic dysfunction is one of the most distress non-motor symptoms in PD. Supine hypertension (SH) and nocturnal hypertension (NH) are rarely reported in early stage PD. It can lead to various serious consequences such as cardiovascular and cerebrovascular events and increased mortality rates.
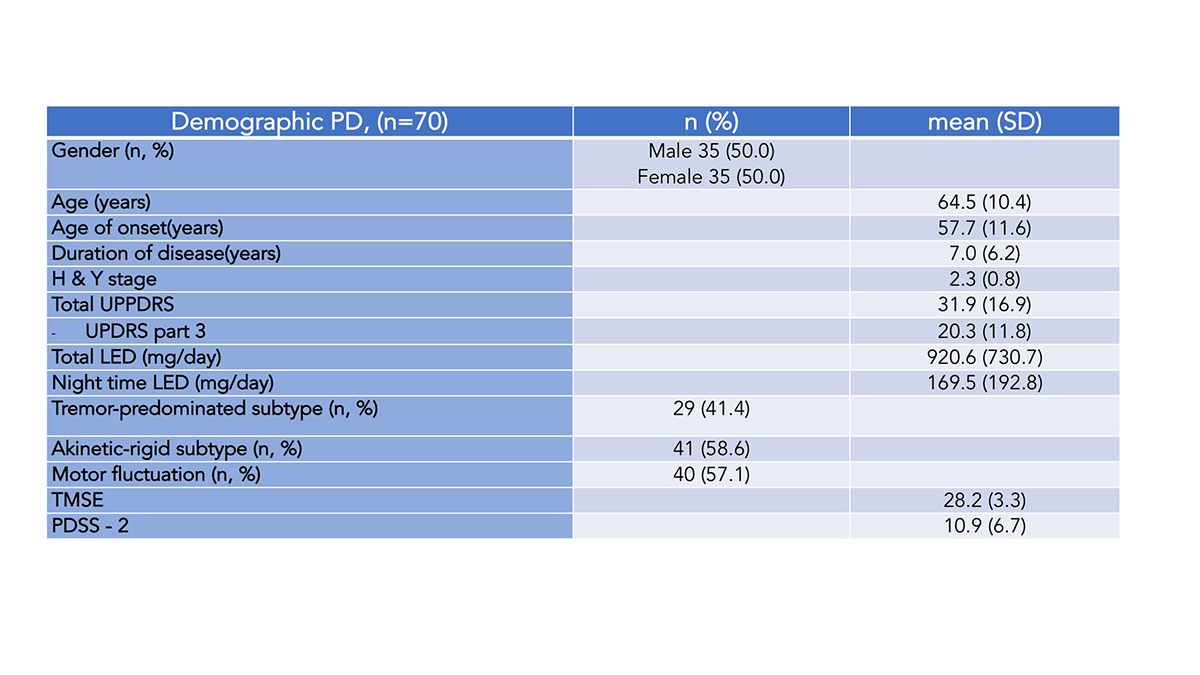
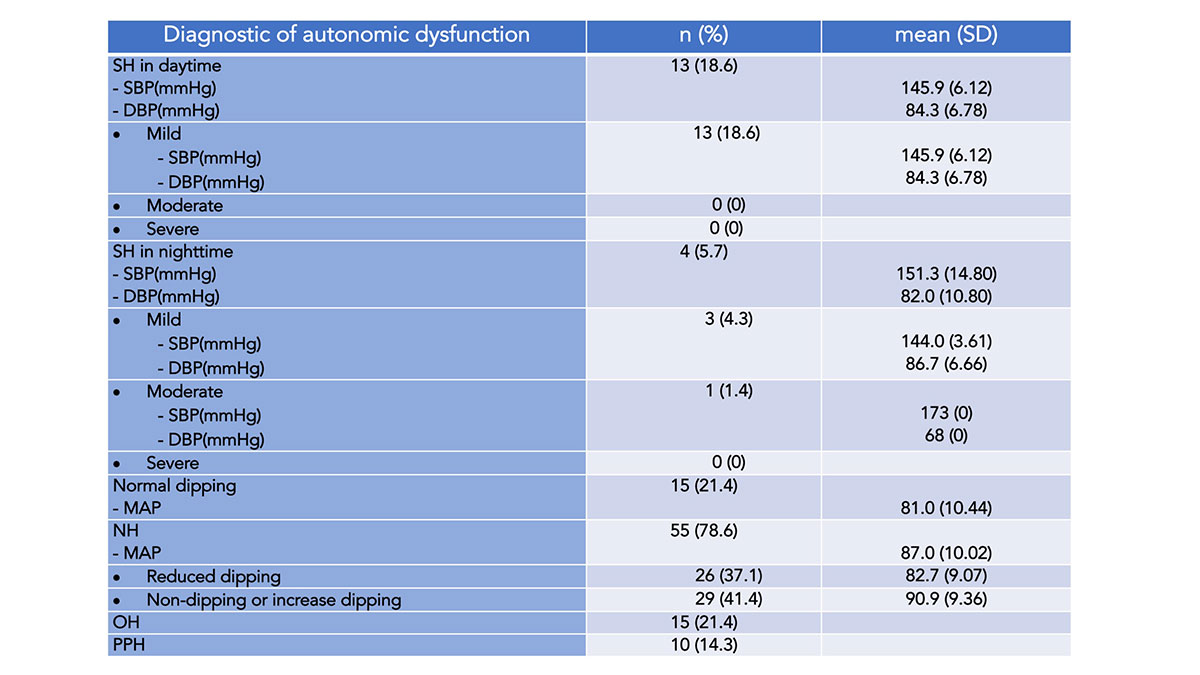
Method: This is an analytic cross-sectional study. 70 PD patients were enrolled in this study to evaluate for SH and NH by measuring BP during day and nighttime by themselves at home with ambulatory BP measurement which has been guarantee validation on ESC 2010. BP was measured in different situations during one day divided into wake-up time, before and after lunch time 90 minutes and 11 PM. And BP was measured in different positions including supine, fowler, right lateral, left lateral and upright position. SH was diagnosed if there were hypertension in the supine position. SH was defined as SBP ≥ 140 and/or DBP ≥ 90 mmHg, measured in the supine position. NH was defined by loss of the physiological nocturnal BP fall at night of ≥ 10% while supine and asleep (dipping).
Results: There were 35 female and 35 male PD in this study. The average age was 64.5 ± 10.4 years. Most of the patients were in moderate stage (H&Y= 2.3). The prevalence of SH in daytime and in nighttime were 18.6% and 5.7%. NH was 78.6%. %. Similarly, the prevalence of OH and PPH were 21.4% and 14.3%. We found the statistically significant correlation between SH in nighttime and duration of disease, orthostatic hypotension and also between NH and RBD. In addition, BP in both lateral positions was statistically significantly less than in supine and fowler position.
Conclusion: The physicians should alert to evaluate for the presence of SH/NH in PD patients especially one who has long disease duration, RBD and orthostatic hypotension. The sleep positions that we should recommend for PD patients can be both lateral positions to decrease the SH and NH.
References: 1. Umehara T, Matsuno H, Toyoda C, Oka H. Clinical characteristics of supine hypertension in de novo Parkinson disease. Clinical Autonomic Research. 2016;26(1):15-21. 2. Fanciulli A, Jordan J, Biaggioni I, Calandra–Buonaura G, Cheshire WP, Cortelli P, et al. Consensus statement on the definition of neurogenic supine hypertension in cardiovascular autonomic failure by the American Autonomic Society (AAS) and the European Federation of Autonomic Societies (EFAS). Clinical Autonomic Research. 2018;28(4):355-62. 3. 1. Kim JS, Park HE, Oh YS, Lee SH, Park JW, Son BC, et al. Orthostatic hypotension and cardiac sympathetic denervation in Parkinson disease patients with REM sleep behavioral disorder. J Neurol Sci. 2016;362:59-63.
To cite this abstract in AMA style:
J. Sringean, R. Hamindra, R. Bhidayasiri. The prevalence of supine hypertension and nocturnal hypertension and the difference of blood pressure in each sleep position in Parkinson’s disease [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/the-prevalence-of-supine-hypertension-and-nocturnal-hypertension-and-the-difference-of-blood-pressure-in-each-sleep-position-in-parkinsons-disease/. Accessed January 4, 2026.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/the-prevalence-of-supine-hypertension-and-nocturnal-hypertension-and-the-difference-of-blood-pressure-in-each-sleep-position-in-parkinsons-disease/