Category: Epidemiology
Objective: To address overall prevalence of Postural deformities(PostD) and each type of PostD (AC, TC, UC, and PS) in PD and healthy volunteers (HVs)
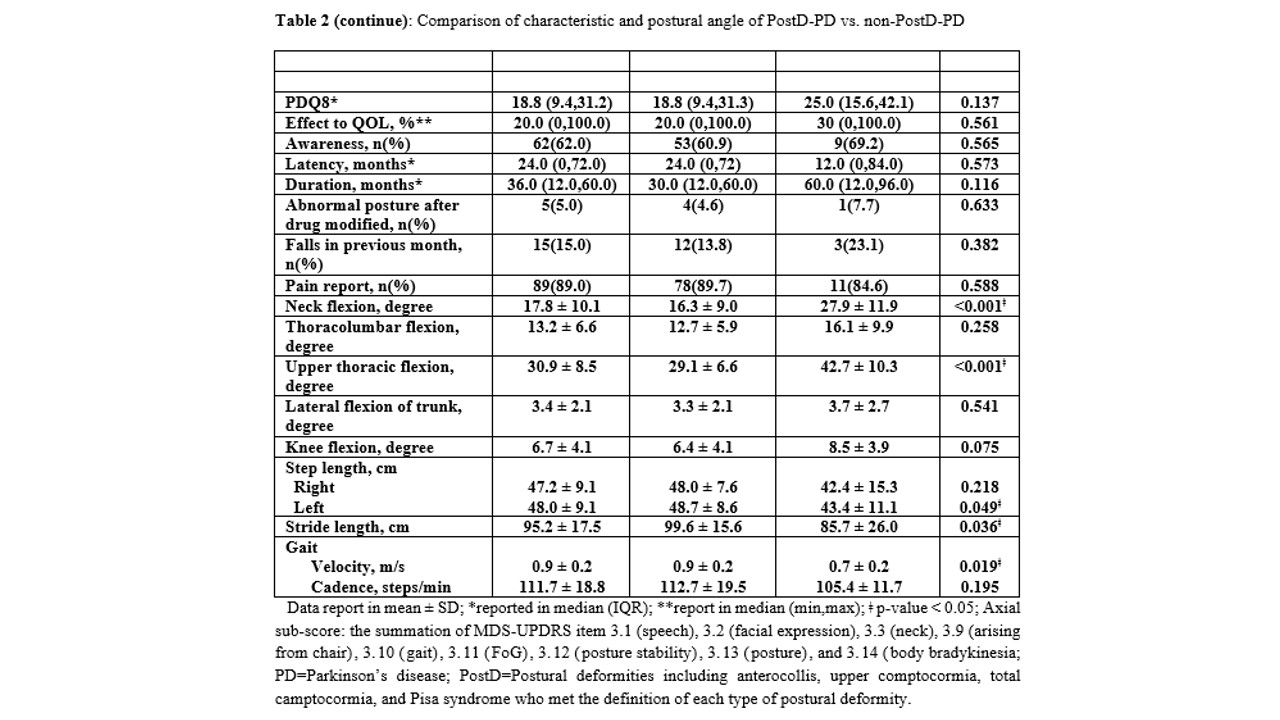
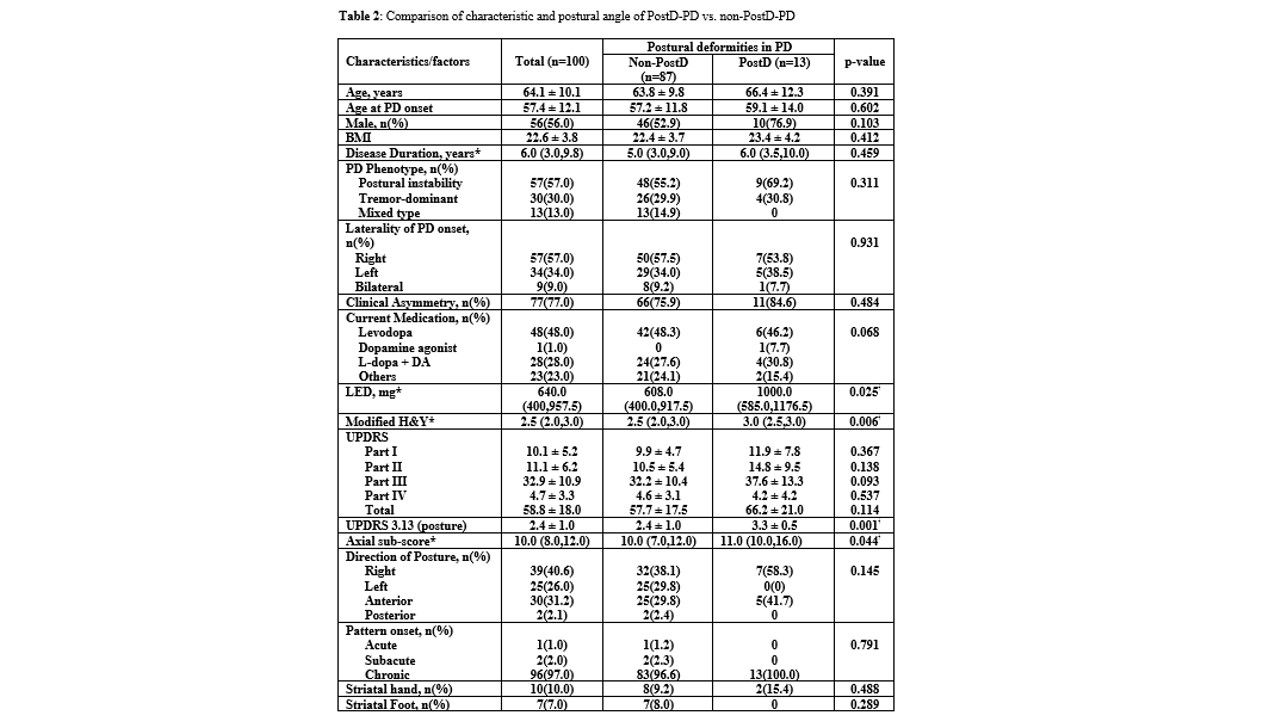
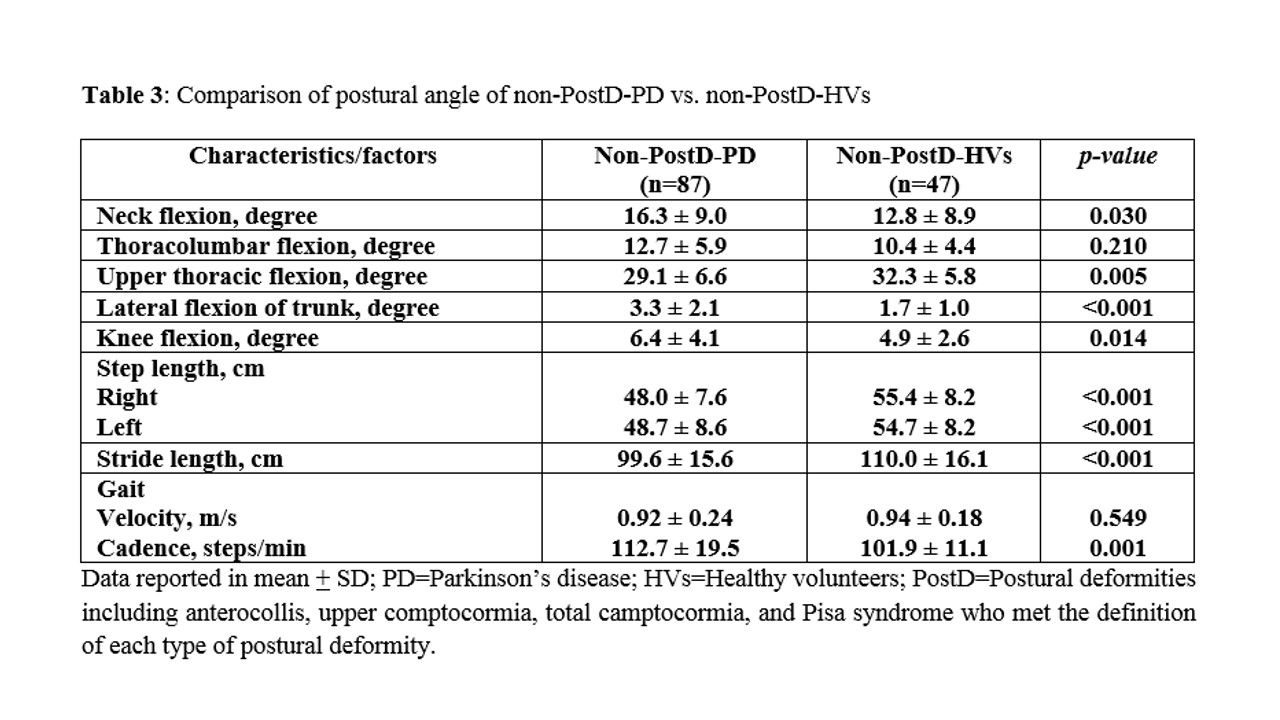
Background: Postural deformities (PostD), including anterocollis (AC), camptocormia (CC), and Pisa syndrome (PS), can be found. They can diminish the quality of life (QoL) in patients with Parkinson’s disease (PD). The primary objective of our study was to address the overall prevalence of PostD in Thai PD patients. We compared clinical characteristics between PostD-PD and PD patients who did not meet the definition of either type of PostD (non-PostD). We compared the degrees of axial deviation for identifying the difference between non-PostD-PD and non-PostD-healthy volunteers (HVs).
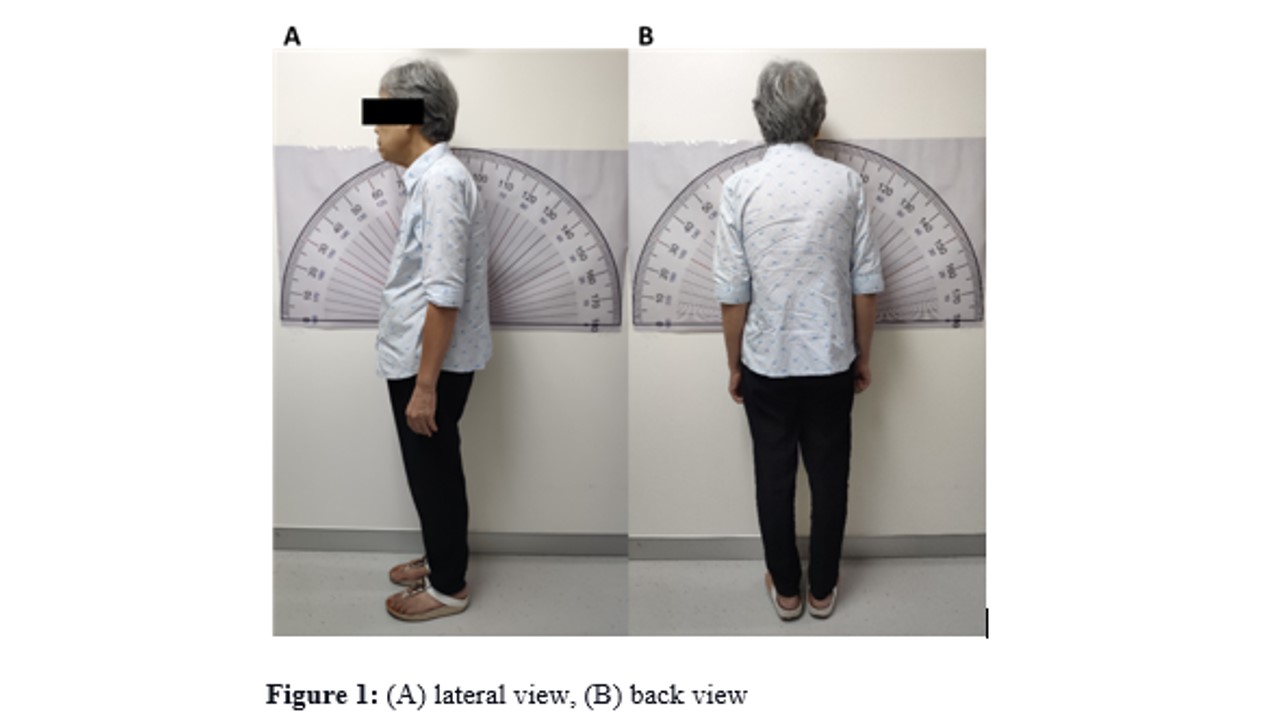
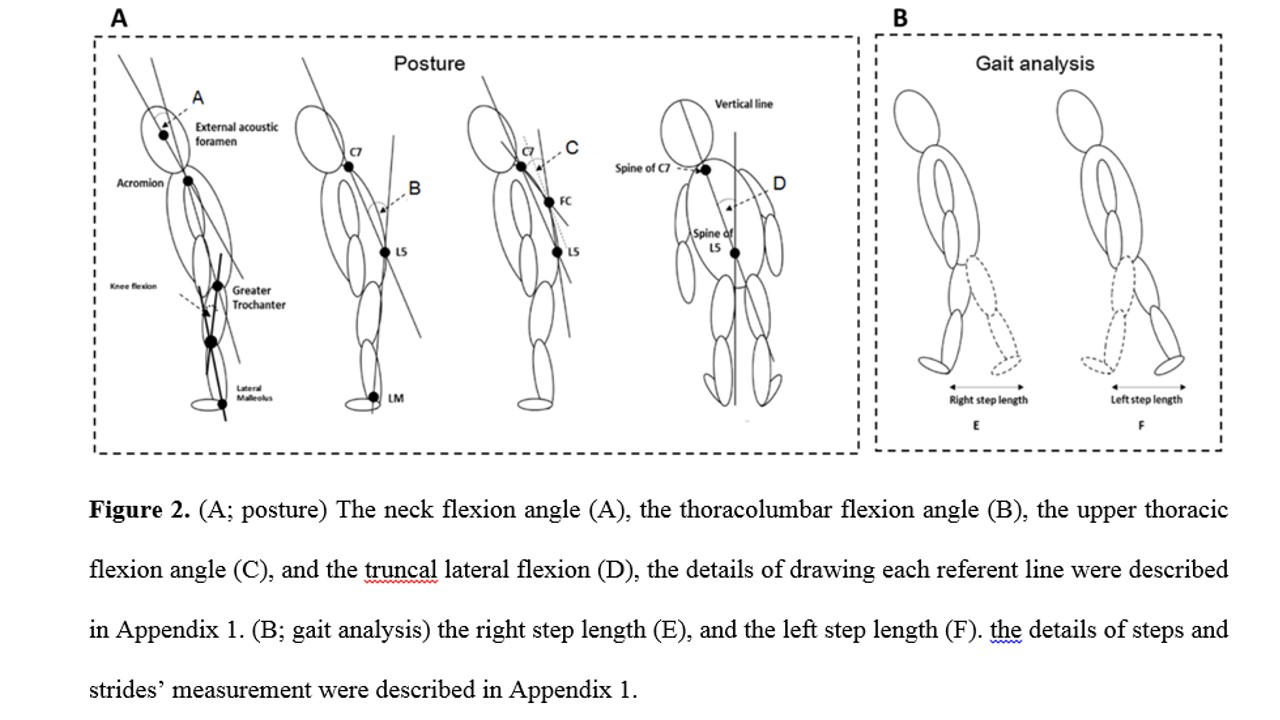
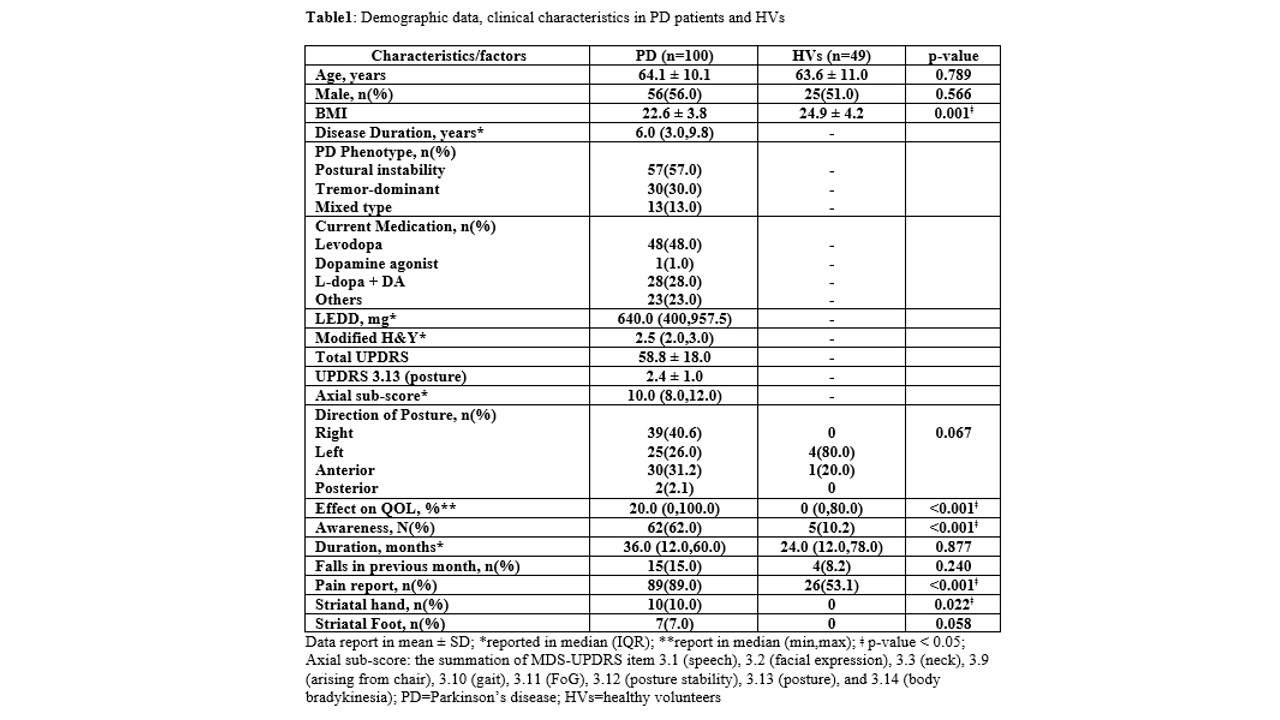
Method: One-hundred Thai PD patients and 49 HVs were recruited. Abnormal postures were evaluated using a computerized measuring program which measured the angles of the neck (NF), upper thoracic, thoracolumbar (TLF), and truncal lateral flexion (LF) from their on-site digital photographs. AC, CC, and PS were defined. Clinical characteristics, MDS-UPDRS, gait velocity, cadence, and QoL, were assessed.
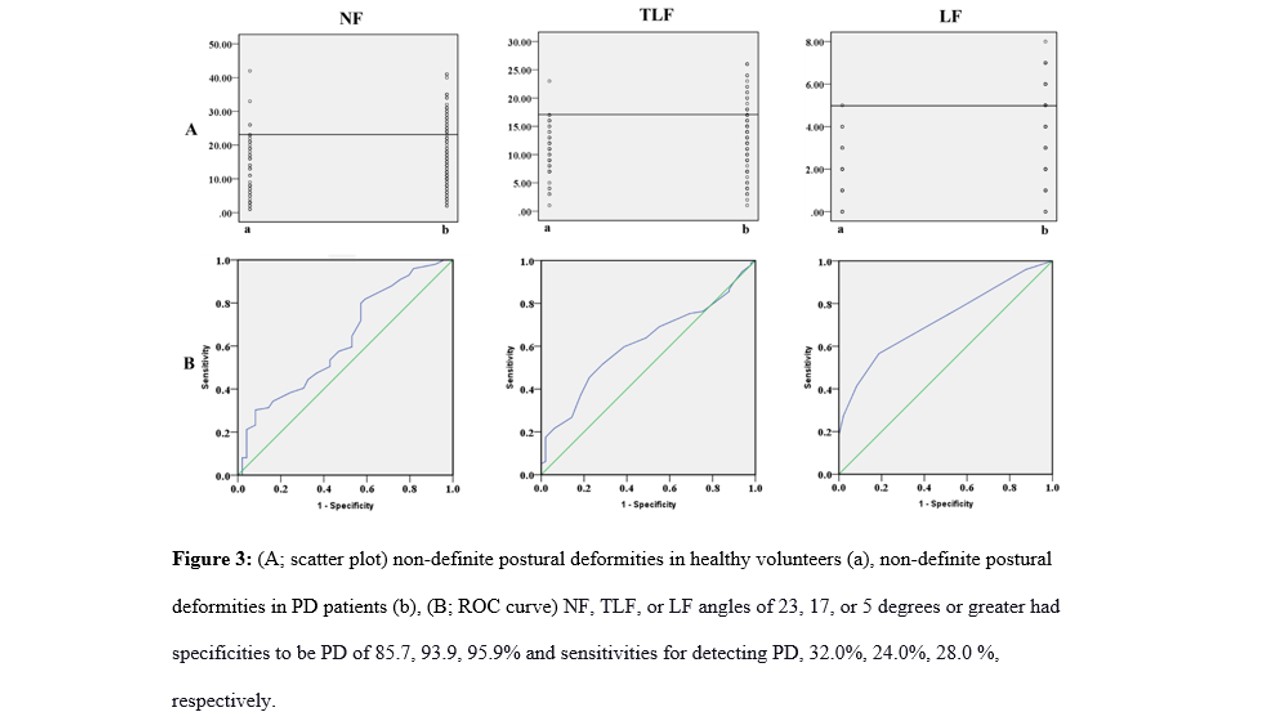
Results: Thirteen of 100 PD patients showed PostD, which mainly CC (n=11), whereas 2 of 49 HVs had PostD. PostD-PD showed significantly more severe motor symptoms than non-PostD-PD (modified H&Y of 3.0 vs. 2.5, MDS-UPDRS (posture) of 3.3 vs. 2.4, a summation of axial sub-scores of 11 vs. 10, and LEDD of 1000 vs. 608 mg). A comparison between non-PostD-PD and non-PostD-HVs showed that NF, TLF, and LF of 23, 17, and 5 degrees or more gave high specificities be PD (85.7, 93.9, and 95.9%, respectively). However, their sensitivities were low.
Conclusion: The most common PostD in Thai PD patients was CC. PostD-PD was associated with high disease severity. Our findings may raise awareness for early detection of PostD in PD, leading physicians to apply an early intervention for falling prevention and improving their QoL.
References: 1. Doherty KM, van de Warrenburg BP, Peralta MC, Silveira-Moriyama L, Azulay JP, Gershanik OS, et al. Postural deformities in Parkinson’s disease. Lancet Neurol. 2011;10(6):538-49. 2. Ashour R, Jankovic J. Joint and skeletal deformities in Parkinson’s disease, multiple system atrophy, and progressive supranuclear palsy. Mov Disord. 2006 Nov;21(11):1856-63. 3. Srivanitchapoom P, Hallett M. Camptocormia in Parkinson’s disease: definition, epidemiology, pathogenesis and treatment modalities. J Neurol Neurosurg Psychiatry. 2016 Jan;87(1):75-85. 4. Pandey S, Kumar H. Assessment of striatal & postural deformities in patients with Parkinson’s disease. Indian J Med Res. 2016;144(5):682-8. 5. Tinazzi M, Gandolfi M, Ceravolo R, Capecci M, Andrenelli E, Ceravolo MG, et al. Postural Abnormalities in Parkinson’s Disease: An Epidemiological and Clinical Multicenter Study. Mov Disord Clin Pract 2019;6(7):576-85. 6. Ando Y. Fujimoto K, Ikeda K, Utsumi H, Okuma Y, Oka H, et al. Postural abnormality in Parkinson’s disease: a large comparative study with general population. Mov Disord Clin Pract 2019;6(3):213-21. 7. Hughes AJ, Daniel SE, Kilford L, Lees AJ. Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinic-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 1992;55(3):181-4. 8. Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 2008;22:41-7. 9. Goetz CG, Poewe W, Rascol O, Sampaio C, Stebbins GT, Counsell C, et al. Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: status and recommendations. Mov Disord 2004;19(9);1020-28. 10. Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, Clarke CE. Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord. (2010) 25:2649-53. 11. Jenkinson C, Fitzpatrick R, Peto V, Greenhall R, Hyman N. The PDQ-8: development and validation of a short-form Parkinson’s disease questionnaire. Psychol Health 1997;12:805–14. 12. Fasano A, Geroin C, Berardelli A, Bloem BR, Espay AJ, Hallett M, et al. Diagnositic criteria for camptocormia in Parkinson’s disease: a consensus-based proposal. Parkinsonism Relat Disord 2018;53:53-7. 13. Parkinson J. An essay on the shaking palsy. 1817. J Neuropsychiatry Clin Neurosci 2002;14(2):223-36. 14. Djaldetti R, Mosberg-Galili R, Sroka H, Merims D, Melamed E. Camptocormia (bent spine) in patients with Parkinson’s disease – characterization and possible pathogenesis of an unusual phenomenon. Mov Disord 1999;14:443-447. 15. Tiple D, Fabbrini G, Colosimo C, et al. Camptocormia in Parkinson disease: an epidemiological and clinical study. J Neurol Neurosurg Psychiatry 2009;80:145-148. 16. Seki M, Takahashi K, Koto A, Mihara B, Morita Y, Isozumi K, et al. Keio Parkinson’s Disease Database. Camptocormia in Japanese patients with Parkinson’s disease: a multicenter study. Mov Disord. 2011;26:2567-71. 17. Oeda T, Umemura A, Tomita S, Hayashi R, Kohsaka M, Sawada H. Clinical factors associated with abnormal postures in Parkinson’s disease. PLoS One 2013;8:e73547. 18. Tramonti C, Di Martino S, Unti E, Frosini D, Bonuccelli U, Rossi B, et al. Gait dynamics in Pisa syndrome and camptocormia: the role of stride length and hip kinematics. Gait Posture 2017;57:130-35.
To cite this abstract in AMA style:
M. Vichutavate, P. Srivanitchapoom. The prevalence and types of postural deformities in Thai patients with Parkinson’s disease: A single-center study [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/the-prevalence-and-types-of-postural-deformities-in-thai-patients-with-parkinsons-disease-a-single-center-study/. Accessed November 8, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/the-prevalence-and-types-of-postural-deformities-in-thai-patients-with-parkinsons-disease-a-single-center-study/