Objective: Identify the unsafe PD patients’ home who had gait problems and provide home modifications.
Background: The motor impairments in PD also involve both appendicular and axial body parts. The axial symptoms or axial motor impairments are one of the major disabling symptoms in PD patients and usually poor response to dopaminergic medications. Gait problems are one of the disabling axial motor symptoms and causing morbidity in PD. More than 50% of PD patients have gait problems when disease progression; ranging from gait instability, shuffling gait, freezing of gait and falling. The majority of falling events occur in patient homes where they use almost of the time there. The inappropriate or unsafe home environment might be the risk of falling.
Method: Ten PD patients who had gait and falling problems were recruited into this study. The demographic data, gait and falling problems, and home-environment problems were assessed by multi-disciplinary team (movement disorder specialists, nurses, architects, and social workers) before and after home modifications. Personalized home environmental adaptations including rail, floor, and bathroom adaptations with a limited budget (1700 $) were applied to each patient’s home.
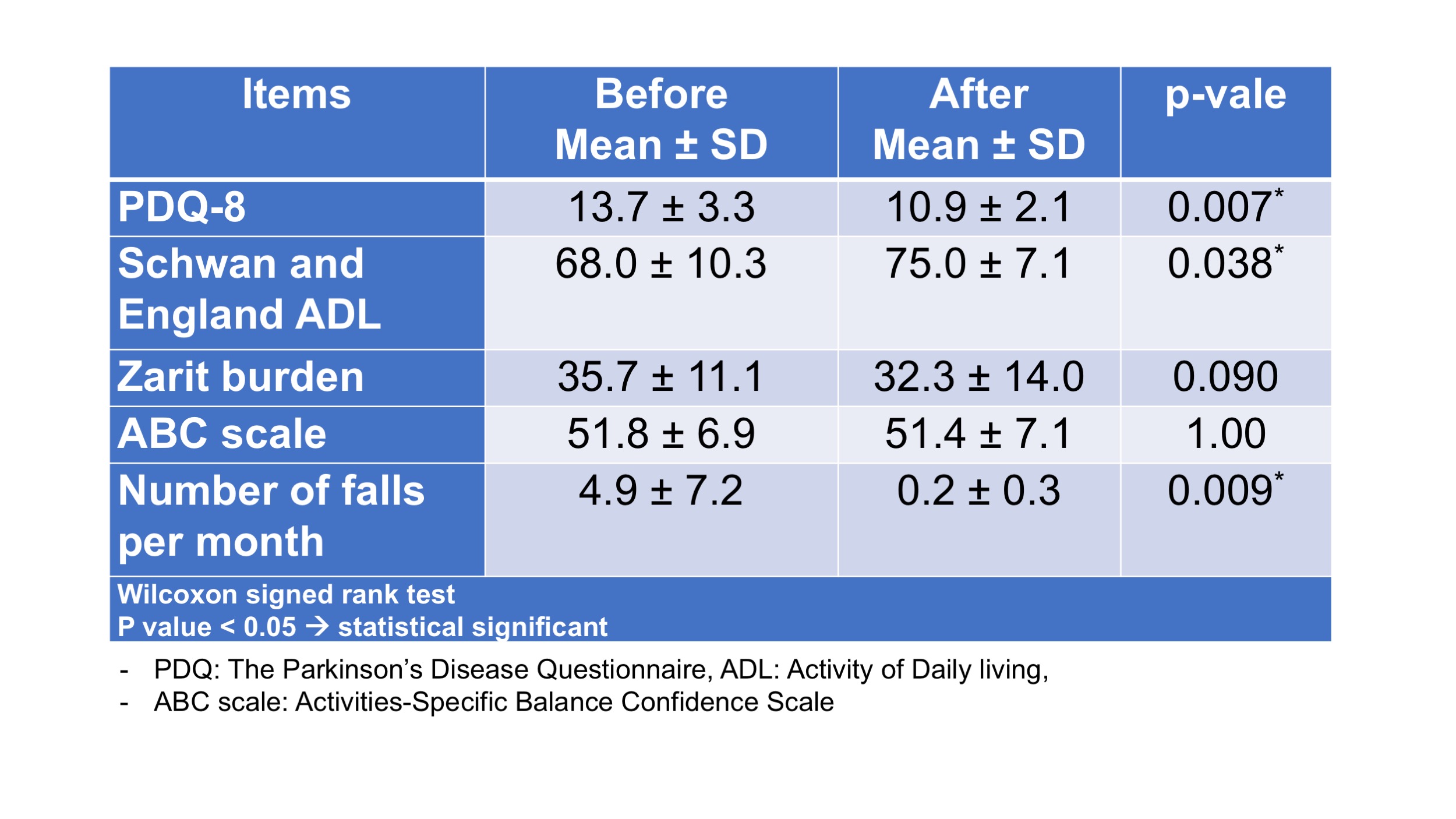
Results: There were 7 males and 3 female PD patients. The mean age and disease duration were 65.6 + 9.9 and 10.4 + 5.3 years. Two patients were H&Y stage 2, 5 patients were H&Y stage 3, and 3 patients were H&Y stage 4. All of them had history of gait problems, freezing of gait, and falling in their home. The mean number of falling in the past month were 4.9 + 7.2 times/month. Seven of them had 2-stoley houses, the others stayed in the apartment, townhouse, and commercial building. After home adaptations were completely done, the falling events were significantly decrease (0.2 + 0.3 times/month, P=0.009). other outcome parameters are shown in table 1.
Conclusion: Personalized home and environmental adaptation is one of the multidisciplinary approaches with effective outcome. Home is the place where PD patient spends most of their time and where the accidents can occur frequently. Especially during the COVID-19 pandemic, people all over the world have to be in their home, home adaptation should be considered as a treatment approach in PD patients.
References: 1.Bhidayasiri R, Jitkritsadakul O, Sringean J, Jantanapornchai T, Kantachadvanich N, Phumphid S, Boonpang K, Pensook S, Aungkab N, Hattori N, Chaudhuri KR. Exploring Bedroom Usability and Accessibility in Parkinson’s Disease (PD): The Utility of a PD Home Safety Questionnaire and Implications for Adaptations. Front Neurol. 2018 May 17;9:360. 2.Ratti PL, Faraci F, Hackethal S, Mascheroni A, Ferlito C, Caverzasio S, et al. A New Perspective, Home-Based Monitoring of Motor Symptoms in Parkinson’s Disease. J Parkinsons Dis 2019;9:803-9. 3. Pelicioni PHS, Menant JC, Latt MD, Lord SR. Falls in Parkinson’s Disease Subtypes: Risk Factors, Locations, and Circumstances. Int J Environ Res Public Health. 2019 Jun 23;16(12):2216.
To cite this abstract in AMA style:
J. Sringean, S. Phumphid, N. Kantachadvanich, R. Bhidayasiri. The effectiveness of home modification on gait and falling episode in Parkinson’s disease (PD) patients. [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/the-effectiveness-of-home-modification-on-gait-and-falling-episode-in-parkinsons-disease-pd-patients/. Accessed December 31, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/the-effectiveness-of-home-modification-on-gait-and-falling-episode-in-parkinsons-disease-pd-patients/