Category: Epidemiology
Objective: To compare the coverage and influencing factors, security, and confidence of COVID-19 vaccination between patients with Parkinson’s disease (PD) and healthy individuals so as to give suggestions for future immunization programs.
Background: PD patients and caregivers have to make a decision on taking COVID-19 vaccination with great caution currently given the lack of evidence-based consensus.
Method: A web-based, nationwide survey was carried out in China from 2021 to 2022. The age and sex-standardized vaccination rate was calculated. Multivariate stepwise logistic regression models were used to estimate the odds ratio (OR) and 95% confidence intervals (CIs) of the influencing factors of vaccination status. We also investigated vaccination safety, willingness, confidence, and reasons for hesitancy with some ad hoc questions.
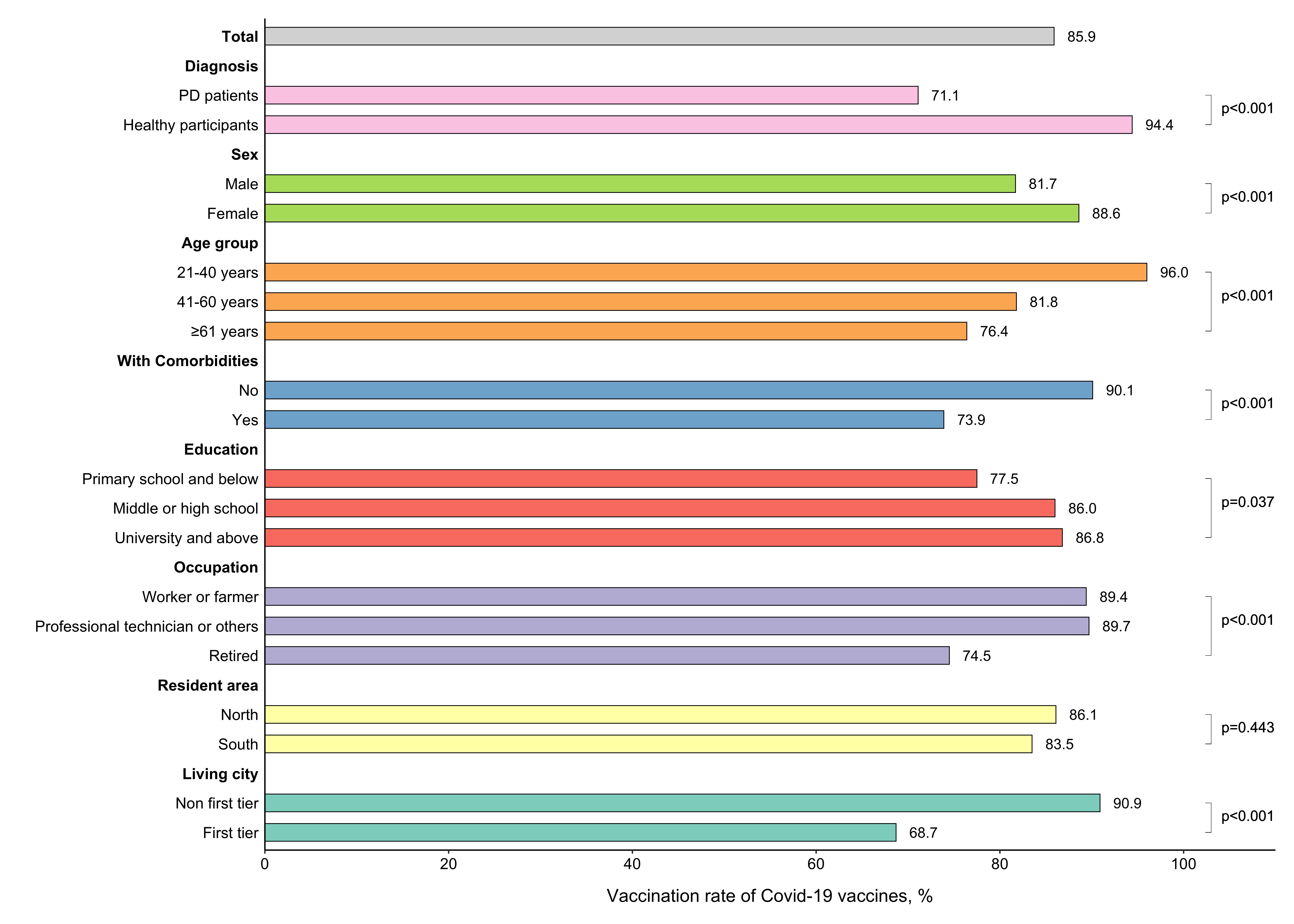
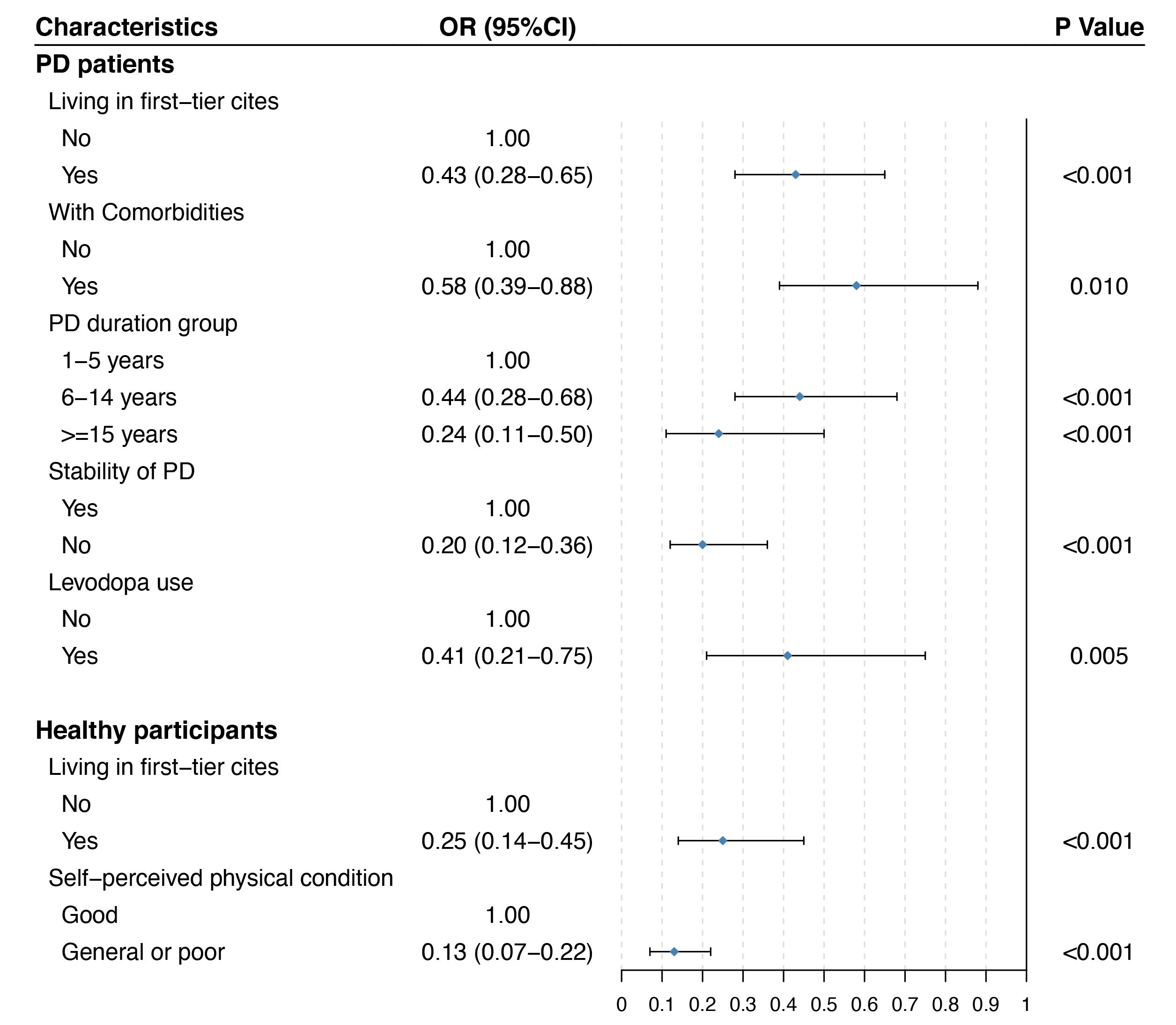
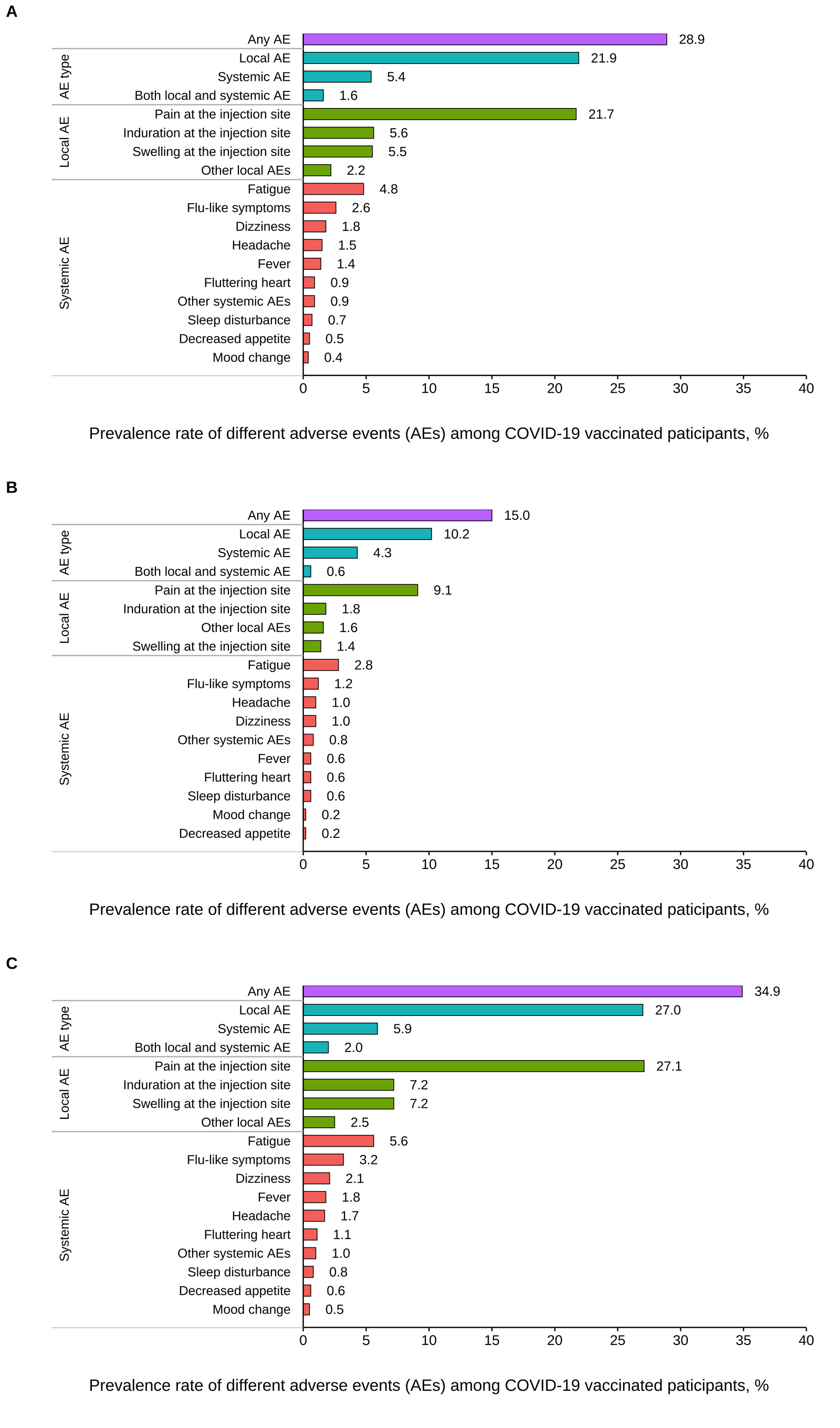
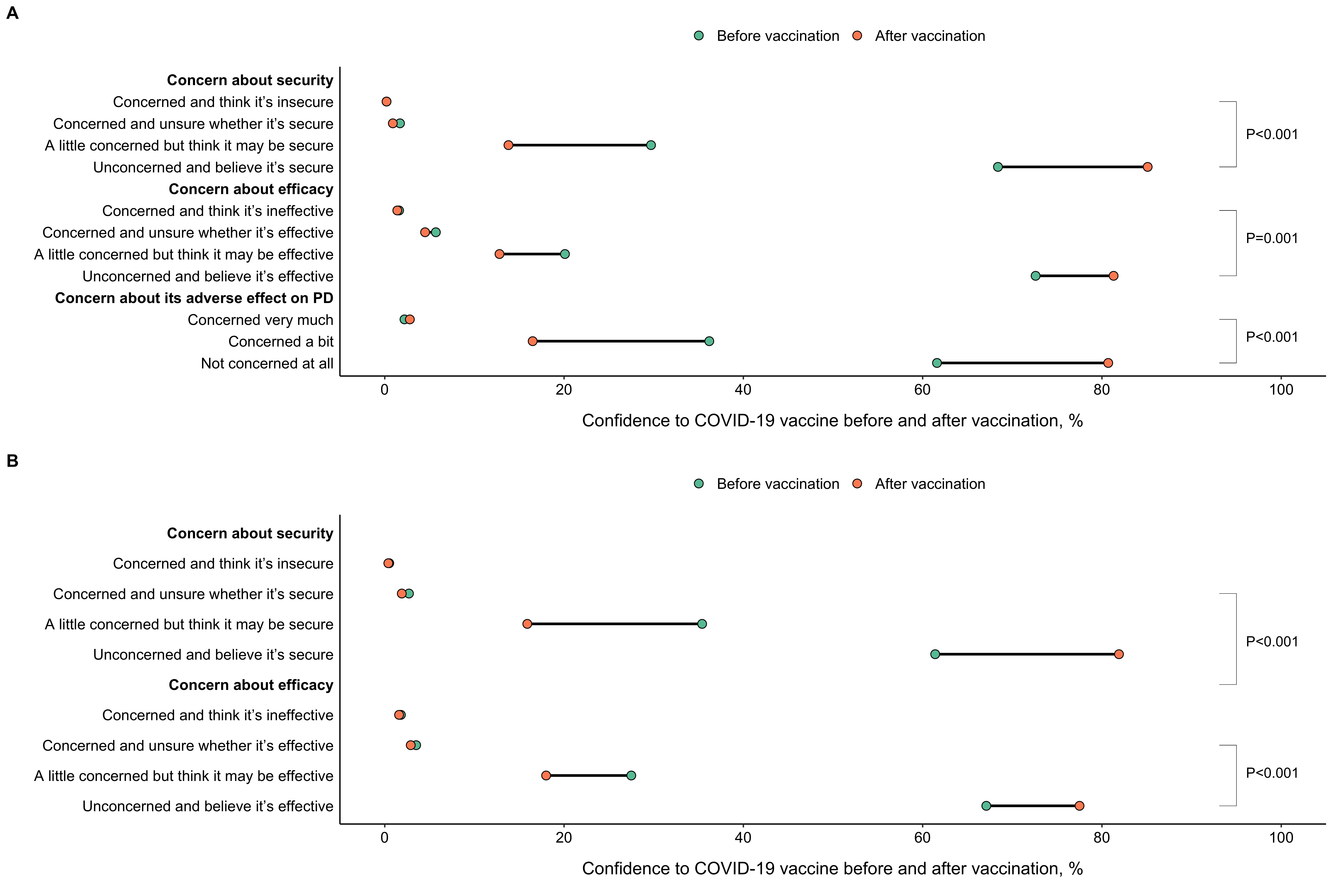
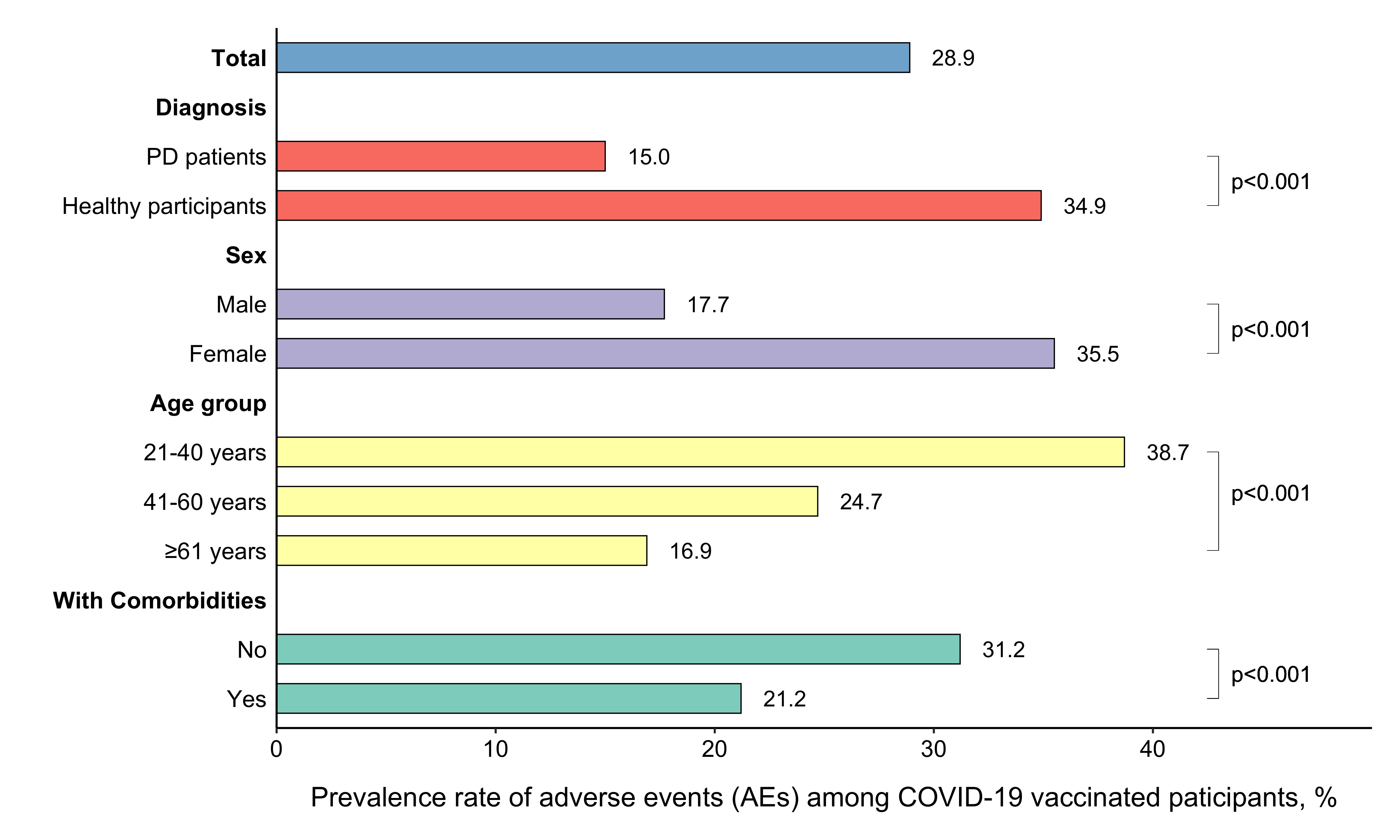
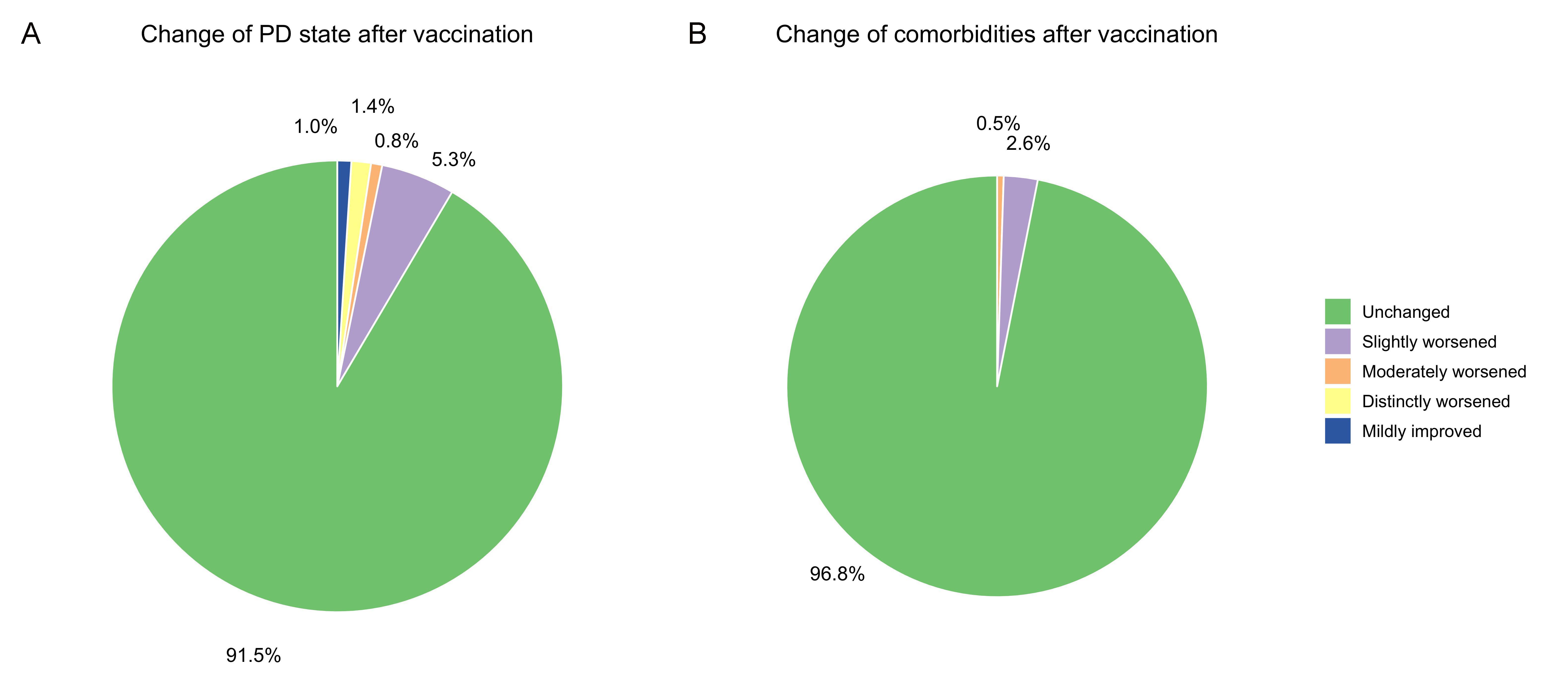
Results: 962 PD patients and 1208 healthy individuals participated in this survey with a vaccination rate of 71.1% vs 94.4% respectively. PD patients living in first-tier cities (OR, 95%CI: 0.43, 0.28-0.65), with comorbidities (0.58, 0.39-0.88), experiencing unstable PD (0.20, 0.12-0.36) with a longer course (0.44, 0.28-0.68; 0.24, 0.11-0.50) and levodopa use (0.41, 0.21-0.75) were less likely to get vaccinated, while healthy individuals living in first-tier cities (0.25, 0.14-0.45) and feeling physically poor (0.13, 0.07-0.22) exhibited a lower vaccination rate. For PD patients, concern about the adverse impact on existing illness and disagreement from doctors were the most common reasons for vaccination hesitancy. Whereas, no evidence was present that they experienced any local or systematic adverse events more frequently or seriously than healthy individuals, or their state of PD and comorbidities was seriously exacerbated after vaccination. A prominent transition from a little concerned to unconcerned about the security and efficacy of vaccines was evident among both two populations from pre-vaccination to post-vaccination.
Conclusion: The COVID-19 vaccination rate was remarkably lower in PD patients than healthy individuals in China. The approved vaccines have shown an acceptable safety profile. Our findings would offer a reference to guide future clinical decision-making of COVID-19 vaccination and improve the immunization management of PD patients.
References: 1. WHO Coronavirus (COVID-19) Dashboard. https://covid19.who.int/. Accessed on 9 Feb 2023.
2. Randolph HE, Barreiro LB. Herd Immunity: Understanding COVID-19. Immunity 2020;52(5):737-741.
3. Zhou Y, Lin Z, Wan X, et al. COVID-19 vaccine acceptance and hesitancy in patients with Parkinson’s disease. Front Public Health 2022;10:977940.
4. Wang Q, Yang L, Jin H, Lin L. Vaccination against COVID-19: A systematic review and meta-analysis of acceptability and its predictors. Prev Med 2021;150:106694.
5. Thunström L, Ashworth M, Finnoff D, Newbold SC. Hesitancy Toward a COVID-19 Vaccine. EcoHealth 2021;18(1):44-60.
6. Chen M, Yuan Y, Zhou Y, et al. Safety of SARS-CoV-2 vaccines: a systematic review and meta-analysis of randomized controlled trials. Infect Dis Poverty 2021;10(1):94.
7. Fendler A, de Vries EGE, GeurtsvanKessel CH, et al. COVID-19 vaccines in patients with cancer: immunogenicity, efficacy and safety. Nat Rev Clin Oncol 2022;19(6):385-401.
8. Wack S, Patton T, Ferris LK. COVID-19 vaccine safety and efficacy in patients with immune-mediated inflammatory disease: Review of available evidence. J Am Acad Dermatol 2021;85(5):1274-1284.
9. Lu L, Zhang Q, Xiao J, et al. COVID-19 vaccine take-up rate and safety in adults with epilepsy: Data from a multicenter study in China. Epilepsia 2022;63(1):244-251.
10. So H, Li T, Chan V, Tam LS, Chan PK. Immunogenicity and safety of inactivated and mRNA COVID-19 vaccines in patients with systemic lupus erythematosus. Ther Adv Musculoskelet Dis 2022;14:1759720X221089586.
11. Capone F, Lucchini M, Ferraro E, et al. Immunogenicity and safety of mRNA COVID-19 vaccines in people with multiple sclerosis treated with different disease-modifying therapies. Neurotherapeutics 2022;19(1):325-333.
12. Soldà G, Barvas E, Lenzi J, et al. Gam-COVID-Vac (Sputnik V) and Pfizer-BioNTech Vaccines Adverse Events following Immunization in Patients Affected by Parkinson’s Disease and Multiple Sclerosis: A Longitudinal Study. Vaccines (Basel) 2022;10(3).
13. Bloem BR, Trenkwalder C, Sanchez-Ferro A, et al. COVID-19 Vaccination for Persons with Parkinson’s Disease: Light at the End of the Tunnel? J Parkinsons Dis 2021;11(1):3-8.
14. Shi Y, Guo M, Yang W, et al. Is SARS-CoV-2 vaccination safe and effective for elderly individuals with neurodegenerative diseases? Expert review of vaccines 2021;20(4):375-383.
15. Schneider SA, Hennig A, Martino D. Relationship between COVID-19 and movement disorders: A narrative review. Eur J Neurol 2022;29(4):1243-1253.
16. Roszmann A, Podlewska AM, Lau YH, Boura I, Hand A. Covid-19 and Parkinson’s disease: Nursing care, vaccination and impact on advanced therapies. Int Rev Neurobiol 2022;165:173-196.
17. Qi S, Yin P, Wang L, et al. Prevalence of Parkinson’s Disease: A Community-Based Study in China. Mov Disord 2021;36(12):2940-2944.
18. Dorsey ER, Constantinescu R, Thompson JP, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology 2007;68(5):384-386.
19. Central Broadcasting Network News. Expert interpretation: why does China vaccine the young before the old? https://baijiahao.baidu.com/s?id=1696246804688555146&wfr=spider&for=pc. Accessed on 9 Feb 2023 (in Chinese).
20. Guang Ming Network News. The first dose of COVID-19 vaccine will be given to 50 million people on January 15. https://m.gmw.cn/baijia/2020-12/21/1301963340.html. Accessed on 9 Feb 2023 (in Chinese).
21. Broadcast Television Network News. Popular science: How many steps does COVID-19 vaccination take? How vaccination strategies differ from country to country? http://www.nbtv.cn/xwdsg/gn/30429261.shtml. Accessed on 9 Feb 2023 (in Chinese).
22. Our World in Data. Coronavirus (COVID-19) Vaccinations. https://ourworldindata.org/covid-vaccinations. Accessed on 9 Feb 2023.
23. The Central People’s Government of the People’s Republic of China. COVID-19 vaccination status. http://www.gov.cn/xinwen/2022-12/24/content_5733396.htm. Accessed on 9 Feb 2023 (in Chinese).
24. National Health Commission. Technical Guidance for COVID-19 Vaccination (1st edition). http://www.gov.cn/xinwen/2021-03/29/content_5596577.htm. Accessed on 9 Feb 2023 (in Chinese).
25. Imbalzano G, Ledda C, Artusi CA, et al. SARS-CoV-2 vaccination, Parkinson’s disease, and other movement disorders: case series and short literature review. Neurol Sci 2022;43(9):5165-5168.
26. Cosentino C, Torres L, Vélez M, et al. SARS-CoV-2 Vaccines and Motor Symptoms in Parkinson’s Disease. Mov Disord 2022;37(1):233.
27. Dulski J, Sławek J. Incidence and characteristics of post-COVID-19 parkinsonism and dyskinesia related to COVID-19 vaccines. Neurol Neurochir Pol 2023.
28. Achiron A, Dolev M, Menascu S, et al. COVID-19 vaccination in patients with multiple sclerosis: What we have learnt by February 2021. Mult Scler 2021;27(6):864-870.
29. Menni C, Klaser K, May A, et al. Vaccine side-effects and SARS-CoV-2 infection after vaccination in users of the COVID Symptom Study app in the UK: a prospective observational study. The Lancet Infectious diseases 2021;21(7):939-949.
30. Rosenblum HG, Gee J, Liu R, et al. Safety of mRNA vaccines administered during the initial 6 months of the US COVID-19 vaccination programme: an observational study of reports to the Vaccine Adverse Event Reporting System and v-safe. The Lancet Infectious Diseases 2022;22(6):802-812.
31. Polack FP, Thomas SJ, Kitchin N, et al. Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine. The New England journal of medicine 2020;383(27):2603-2615.
32. Elnaem MH, Mohd Taufek NH, Ab Rahman NS, et al. COVID-19 Vaccination Attitudes, Perceptions, and Side Effect Experiences in Malaysia: Do Age, Gender, and Vaccine Type Matter? Vaccines (Basel) 2021;9(10).
33. Wang J, Tong Y, Li D, Li J, Li Y. The Impact of Age Difference on the Efficacy and Safety of COVID-19 Vaccines: A Systematic Review and Meta-Analysis. Front Immunol 2021;12:758294.
34. Huang P, Zhang LY, Tan YY, Chen SD. Links between COVID-19 and Parkinson’s disease/Alzheimer’s disease: reciprocal impacts, medical care strategies and underlying mechanisms. Transl Neurodegener 2023;12(1):5.
35. Lau YH, Lau KM, Ibrahim NM. Management of Parkinson’s Disease in the COVID-19 Pandemic and Future Perspectives in the Era of Vaccination. J Mov Disord 2021;14(3):177-183.
36. Russo AG, Decarli A, Valsecchi MG. Strategy to identify priority groups for COVID-19 vaccination: A population based cohort study. Vaccine 2021;39(18):2517-2525.
37. Phanhdone T, Drummond P, Meisel T, et al. Barriers to Vaccination Among People with Parkinson’s Disease and Implications for COVID-19. J Parkinsons Dis 2021;11(3):1057-1065.
38. Wong MCS, Wong ELY, Huang J, et al. Acceptance of the COVID-19 vaccine based on the health belief model: A population-based survey in Hong Kong. Vaccine 2021;39(7):1148-1156.
39. The Central People’s Government of the People’s Republic of China. Notice on further optimizing the implementation of the prevention and control measures of COVID-19 epidemic. http://www.gov.cn/xinwen/2022-12/07/content_5730443.htm. Accessed on 9 Feb 2023 (in Chinese).
To cite this abstract in AMA style:
C. Han, Z. Zhao, J. Ma. The comparison of vaccination rate, health impact, and confidence of COVID-19 vaccines between patients with Parkinson’s disease and healthy population: evidence from a large multicenter survey in China [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/the-comparison-of-vaccination-rate-health-impact-and-confidence-of-covid-19-vaccines-between-patients-with-parkinsons-disease-and-healthy-population-evidence-from-a-large-multicenter-surve/. Accessed March 6, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/the-comparison-of-vaccination-rate-health-impact-and-confidence-of-covid-19-vaccines-between-patients-with-parkinsons-disease-and-healthy-population-evidence-from-a-large-multicenter-surve/