Session Information
Date: Thursday, June 8, 2017
Session Title: Other
Session Time: 1:15pm-2:45pm
Location: Exhibit Hall C
Objective: This study aimed: (i) to identify the best combination of clinical scales and walking measures to predict falls in people with Parkinson’s disease (PD) after a four-, six-, and 12-month prospective follow-up period; (ii) and to identify the circumstances of falls reported.
Background: Fall occurrence is a major problem for people with PD. Exploring the length of the prospective follow-up period in order to optimize the prediction of falls in PD is particularly important because it has potential to guide the frequency for fall risk assessment that patients should be submitted to.
Methods: Fifty-eight patients with idiopathic PD completed the baseline clinical (rating scales for PD) and walking assessments (spatiotemporal parameters of gait and obstacle avoidance) and reported falls for 12 months. Falls were classified according to the circumstances they occurred. The participants were classified as a ‘faller’ if they suffered at least two falls during the periods of interest. The ability of each outcome measure and combinations to predict falls at four, six, and 12 months was assessed using receiver operating characteristic curve analyses. Top predictors were combined and for each hit cutoff value one point was added at the final score of each combination.
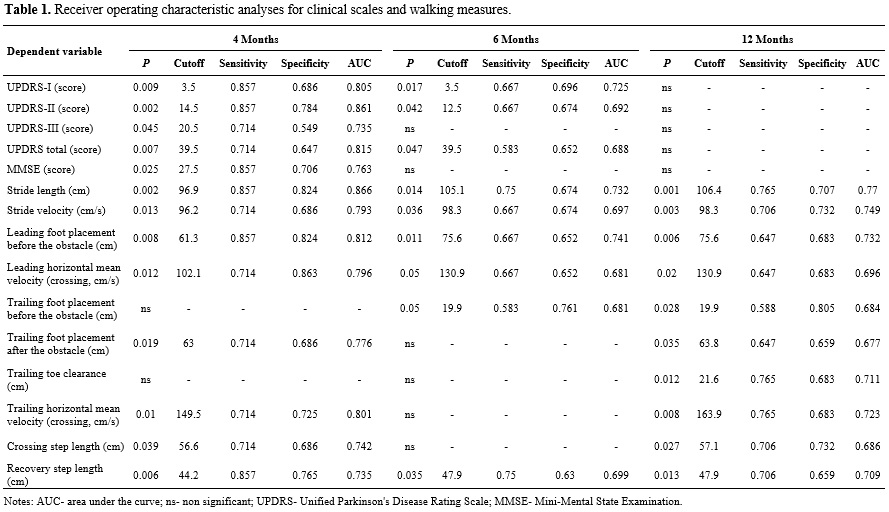
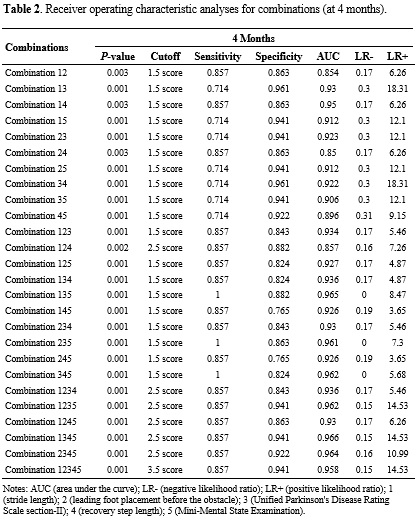
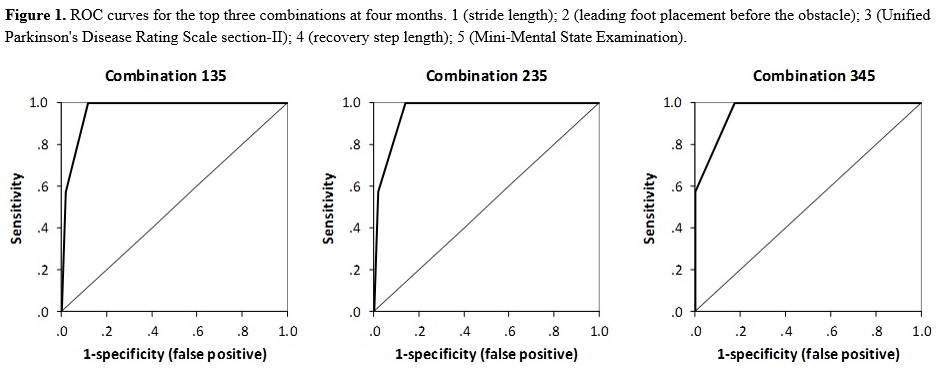
Results: Thirty-one individuals (53.4%) felt at least once during the 12-month fall assessment (fallers: 7 individuals at four months, 12 individuals at six months, and 17 individuals at 12 months). The area under the curve, sensitivity, and specificity scores were highest at four months [table1]. Three combinations of predictors were able to identify 100% of fallers patients at four months, with false positive rates between 11.8% and 17.6% [table2]. The best combination included the UPDRS section II, the Mini-Mental State Examination and stride length [figure1]. Most falls occurred in the morning (57%), under good effect of medication (82%), in a domestic indoor environment (56%). The major causes of falls were loss of balance with no apparent cause (42%) and tripping (39%).
Conclusions: These findings suggest that the combination of clinical scales and walking measures should be used in clinical practice to assess the possibility of people with PD become fallers in the next four months. Fall phenotype observed support preventive actions to reduce fall occurrence in PD.
To cite this abstract in AMA style:
R. Vitório, R. Moraes, A. Baptista, E. Lirani-Silva, L. Simieli, D. Orcioli-Silva, F. Barbieri, L. Gobbi. The combination of clinical scales and walking measures to predict falls in Parkinson’s disease: Does the length of the prospective follow-up period matter? [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/the-combination-of-clinical-scales-and-walking-measures-to-predict-falls-in-parkinsons-disease-does-the-length-of-the-prospective-follow-up-period-matter/. Accessed December 31, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/the-combination-of-clinical-scales-and-walking-measures-to-predict-falls-in-parkinsons-disease-does-the-length-of-the-prospective-follow-up-period-matter/