Category: Parkinson's Disease: Non-Motor Symptoms
Objective: This study investigates the association between pain and motor symptom severity (MSS) in PD patients.
Background: Parkinson’s Disease (PD) is the second most common neurodegenerative disorder characterized by motor symptoms like bradykinesia, tremor, rigidity, and postural instability. These symptoms of PD severely impact physical abilities and functional independence. Pain, which also affects 67.6% of PD patients, varies in form and presentation and is often invisible and underdiagnosed.
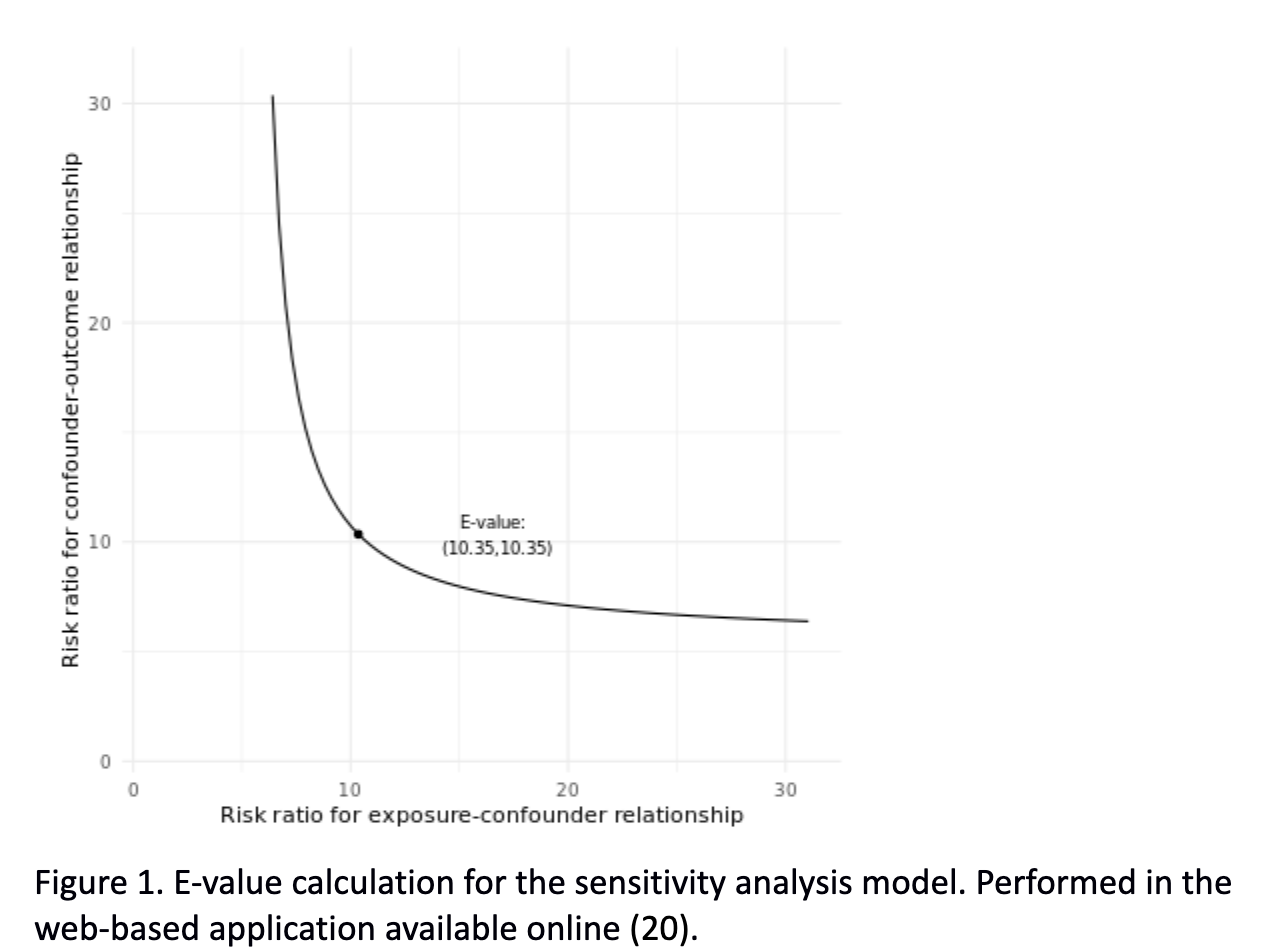
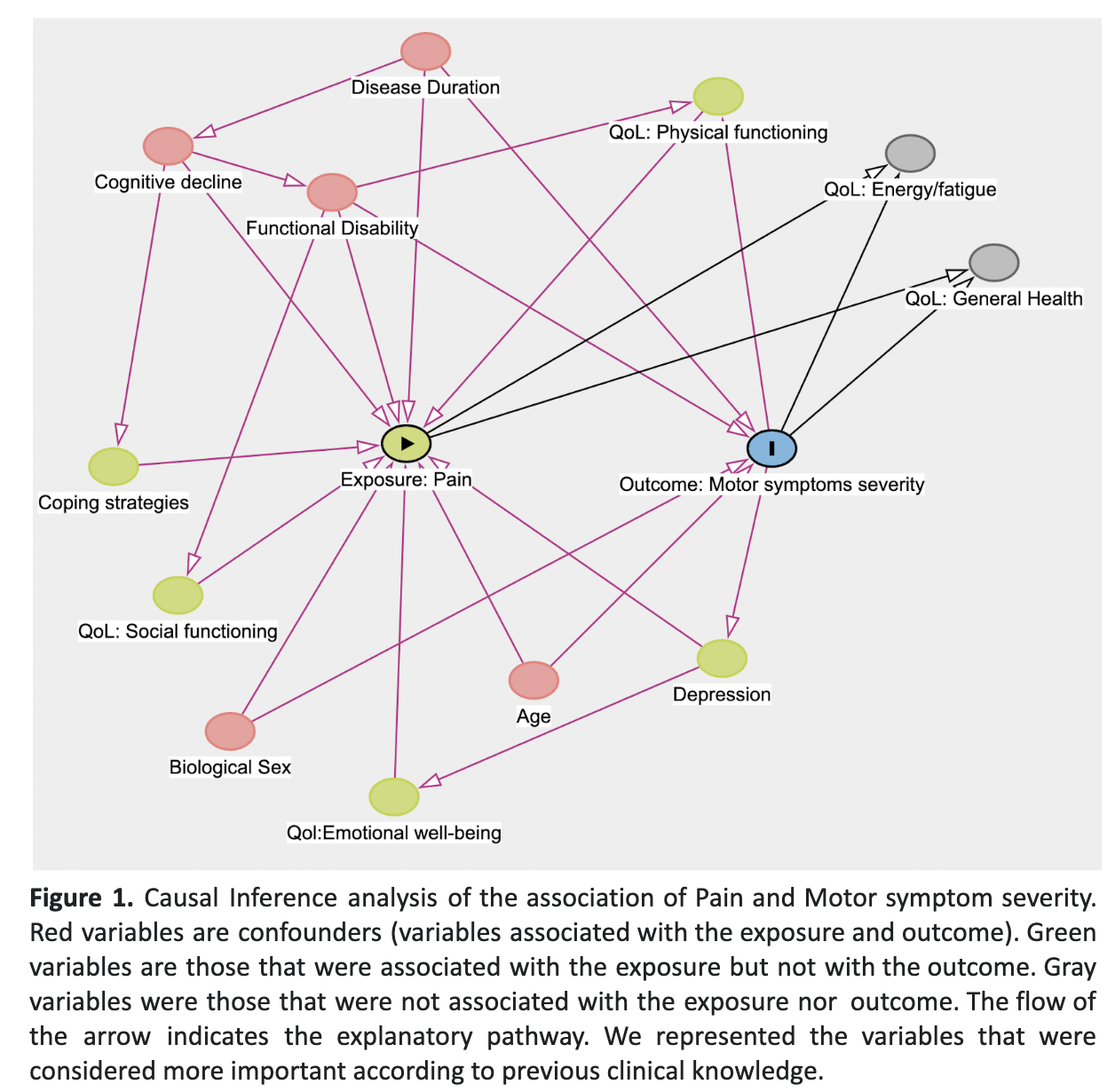
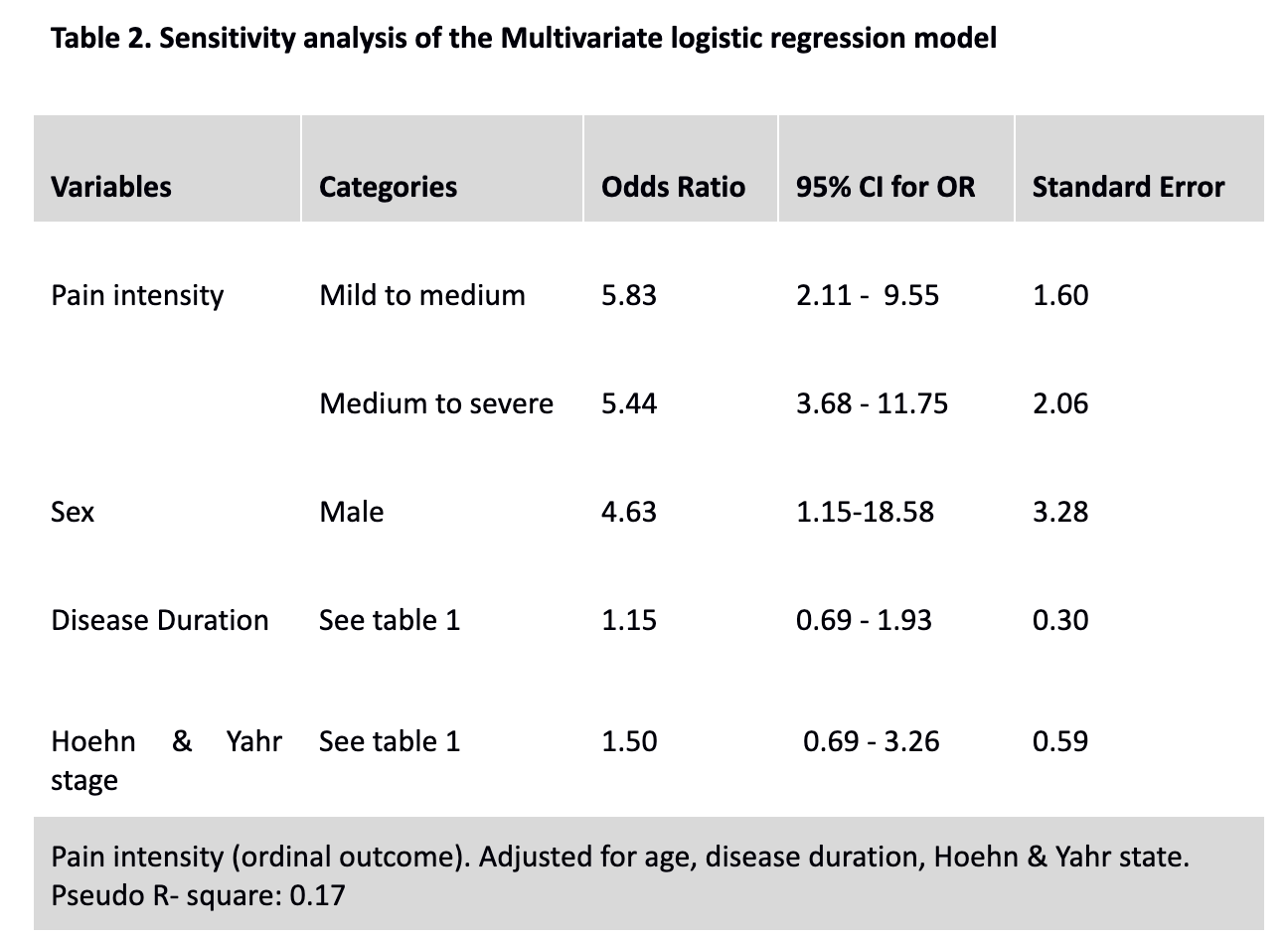
Method: This analysis used data from a cross-sectional study on 52 Parkinson’s Disease (PD) patients conducted at Jena University Hospital, Germany. The dataset, available on Dryad, included demographics, clinical reports, assessments of coping strategies, quality of life, and pain. Descriptive statistics, a bivariate analysis, and an ordinal logistic regression model were executed to explore the association between pain and MSS. A causal inference analysis identified potential confounders and a sensitivity analysis assessed the impact of using pain intensity as an outcome [Figure 1]. The E-value was calculated to evaluate the strength of the association an unmeasured confounder needs to nullify the observed association [Figure 2].
Results:
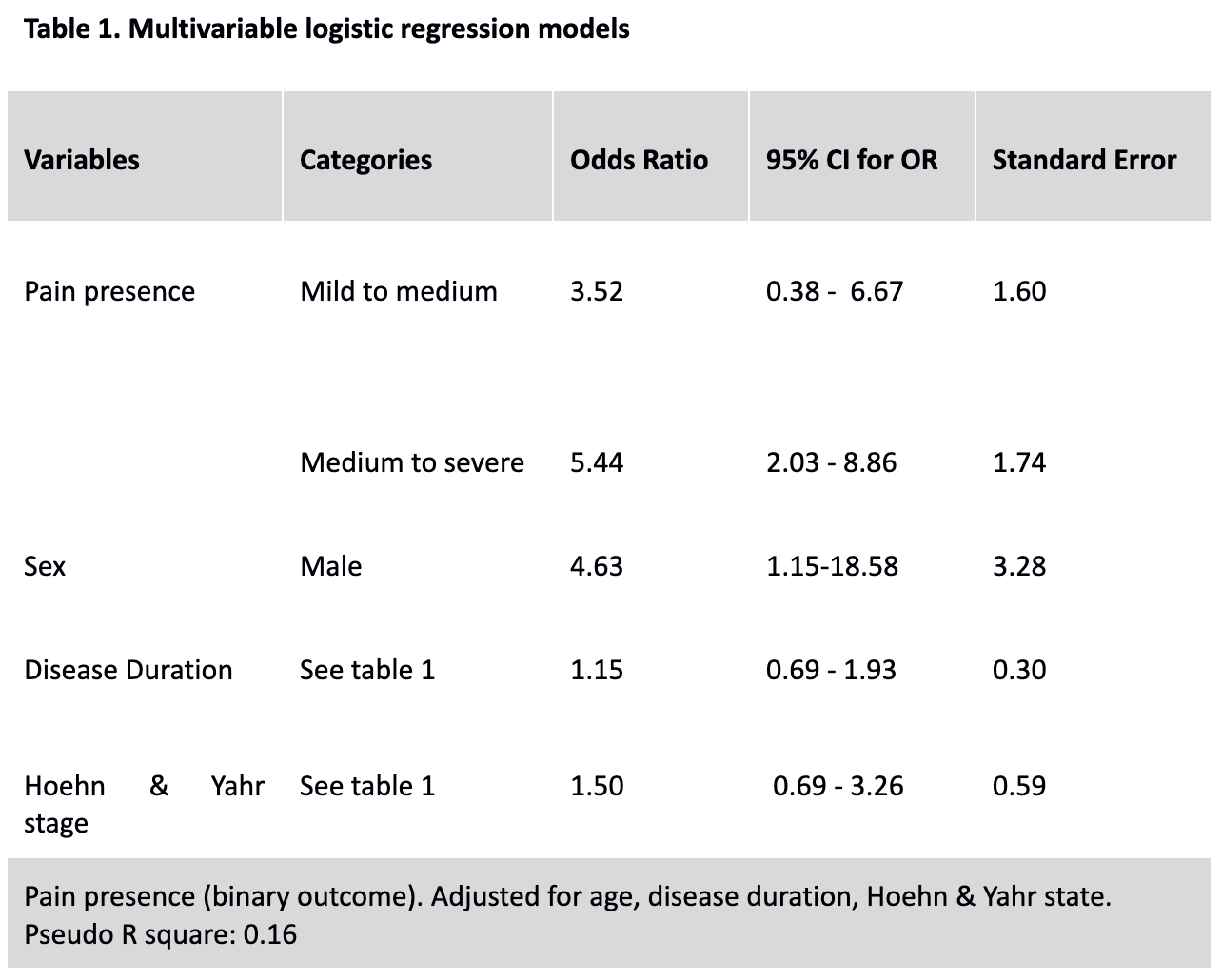
50 Parkinson’s Disease (PD) patients were included, with 64% of these patients being male, with an average age of 76.1 years. The sample included 20 patients without pain and 30 with pain. The bivariate analysis did not identify significant differences between the pain and no-pain groups in disease duration, cognitive function, and non-motor symptoms. However, significant differences between groups emerged in motor symptom severity, coping strategies, and several SF-36 domains (Physical and Social Functioning, Role Functioning, Energy/Fatigue, Pain, General Health, and Health Change). In the multivariate analysis [table2], the estimate of Pain presence for low to medium motor symptom severity was OR 3.52 (95% CI:0.38 – 6.67) and the estimate for medium to severe was OR 5.44 (95% CI:2.03 – 8.86). In addition, being a male was associated with increased motor symptom severity OR 4.63 (95% CI:1.15-18.58).
Conclusion: Pain and MSS are associated, showing a stronger association in patients progressing from medium to severe MSS, following a dose-response relation. Prospective studies are needed to verify these findings.
Figure 2
Figure 1
Table 1
Table 2
References: 1. Parkinson disease [Internet]. [cited 2023 Nov 11]. Available from: https://www.who.int/news-room/fact-sheets/detail/parkinson-disease
2. Dorsey ER, Constantinescu R, Thompson JP, Biglan KM, Holloway RG, Kieburtz K, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007 Jan 30;68(5):384–6.
3. Mettler FA. The substantia nigra and parkinsonism. Trans Am Neurol Assoc. 1964;89:68–73.
4. Den Oudsten BL, Van Heck GL, De Vries J. Quality of life and related concepts in Parkinson’s disease: a systematic review. Mov Disord. 2007 Aug 15;22(11):1528–37.
5. Markovich S, Schwab RS. Prognosis and progression of Parkinson’s disease in patients under medical treatment. AMA Arch Neurol Psychiatry. 1953 Feb;69(2):252–4.
6. Marttila RJ, Rinne UK. Disability and progression in Parkinson’s disease. Acta Neurol Scand. 1977 Aug;56(2):159–69.
7. Kalia LV, Lang AE. Parkinson’s disease. Lancet. 2015 Aug 29;386(9996):896–912.
8. Post B, Merkus MP, de Haan RJ, Speelman JD, CARPA Study Group. Prognostic factors for the progression of Parkinson’s disease: a systematic review. Mov Disord. 2007 Oct 15;22(13):1839–51; quiz 1988.
9. Broen MPG, Braaksma MM, Patijn J, Weber WEJ. Prevalence of pain in Parkinson’s disease: a systematic review using the modified QUADAS tool. Mov Disord. 2012 Apr;27(4):480–4.
10. Thompson T, Gallop K, Correll CU, Carvalho AF, Veronese N, Wright E, et al. Pain perception in Parkinson’s disease: A systematic review and meta-analysis of experimental studies. Ageing Res Rev. 2017 May;35:74–86.
11. Defazio G, Antonini A, Tinazzi M, Gigante AF, Pietracupa S, Pellicciari R, et al. Relationship between pain and motor and non-motor symptoms in Parkinson’s disease. Eur J Neurol. 2017 Jul;24(7):974–80.
12. Tinazzi M, Del Vesco C, Fincati E, Ottaviani S, Smania N, Moretto G, et al. Pain and motor complications in Parkinson’s disease. J Neurol Neurosurg Psychiatry. 2006 Jul;77(7):822–5.
13. de Mattos DC, Meziat Filho NA, Pedron CA, Vasconcellos LF, Nogueira LAC, de Oliveira LAS. Pain Characteristics and Their Relationship With Motor Dysfunction in Individuals With Parkinson Disease-A Cross-Sectional Study. Pain Pract. 2019 Sep;19(7):732–9.
14. Buhmann C, Kassubek J, Jost WH. Management of Pain in Parkinson’s Disease. J Parkinsons Dis. 2020;10(s1):S37–48.
15. Tai YC, Lin CH. An overview of pain in Parkinson’s disease. Clin Park Relat Disord. 2020;2:1–8.
16. Prell T, Liebermann JD, Mendorf S, Zipprich HM. Data on pain coping strategies and their association with quality of life in people with Parkinson’s disease: A cross-sectional study. Data Brief. 2022 Jun;42:108288.
17. Prell T. Pain coping strategies and their association with quality of life in people with Parkinson’s Disease: a Cross-Sectional study [Internet]. Dryad; [cited 2023 Nov 14]. Available from: http://datadryad.org/stash/dataset/doi%253A10.5061%252Fdryad.2280gb5s7
18. Martínez-Martín P, Rodríguez-Blázquez C, Mario Alvarez, Arakaki T, Arillo VC, Chaná P, et al. Parkinson’s disease severity levels and MDS-Unified Parkinson’s Disease Rating Scale. Parkinsonism Relat Disord. 2015 Jan;21(1):50–4.
19. VanderWeele TJ, Ding P. Sensitivity Analysis in Observational Research: Introducing the E-Value. Ann Intern Med. 2017 Aug 15;167(4):268–74.
20. Mathur MB, Ding P, Riddell CA, VanderWeele TJ. Web Site and R Package for Computing E-values. Epidemiology. 2018 Sep;29(5):e45–7.
21. Li J, Zhu BF, Gu ZQ, Zhang H, Mei SS, Ji SZ, et al. Musculoskeletal Pain in Parkinson’s Disease. Front Neurol. 2021;12:756538.
22. Nolano M, Provitera V, Estraneo A, Selim MM, Caporaso G, Stancanelli A, et al. Sensory deficit in Parkinson’s disease: evidence of a cutaneous denervation. Brain. 2008 Jul;131(Pt 7):1903–11.
23. Lin CH, Chao CC, Wu SW, Hsieh PC, Feng FP, Lin YH, et al. Pathophysiology of Small-Fiber Sensory System in Parkinson’s Disease: Skin Innervation and Contact Heat Evoked Potential. Medicine . 2016 Mar;95(10):e3058.
24. Sharma SK. Skin nerve α-synuclein deposits: a biomarker for idiopathic Parkinson disease. Neurology. 2014 Oct 21;83(17):1582.
25. Wang N, Gibbons CH, Lafo J, Freeman R. α-Synuclein in cutaneous autonomic nerves. Neurology. 2013 Oct 29;81(18):1604–10.
26. Cong S, Xiang C, Zhang S, Zhang T, Wang H, Cong S. Prevalence and clinical aspects of depression in Parkinson’s disease: A systematic review and meta‑analysis of 129 studies. Neurosci Biobehav Rev. 2022 Oct;141:104749.
27. Starkstein SE, Preziosi TJ, Robinson RG. Sleep disorders, pain, and depression in Parkinson’s disease. Eur Neurol. 1991;31(6):352–5.
28. Goetz CG, Wilson RS, Tanner CM, Garron DC. Relationships among pain, depression, and sleep alterations in Parkinson’s disease. Adv Neurol. 1987;45:345–7.
29. Martin SL, Jones AKP, Brown CA, Kobylecki C, Silverdale MA. A neurophysiological investigation of anticipation to pain in Parkinson’s disease. Eur J Neurosci. 2020 Jan;51(2):611–27.
30. Pautrat A, Rolland M, Barthelemy M, Baunez C, Sinniger V, Piallat B, et al. Revealing a novel nociceptive network that links the subthalamic nucleus to pain processing. Elife [Internet]. 2018 Aug 28;7. Available from: http://dx.doi.org/10.7554/eLife.36607
31. Wang ZM, Wei PH, Shan Y, Han M, Zhang M, Liu H, et al. Identifying and characterizing projections from the subthalamic nucleus to the cerebellum in humans. Neuroimage. 2020 Apr 15;210:116573.
32. Santos AN, Kherif F, Melie-Garcia L, Lutti A, Chiappini A, Rauschenbach L, et al. Parkinson’s disease may disrupt overlapping subthalamic nucleus and pallidal motor networks. Neuroimage Clin. 2023 May 13;38:103432.
33. Cury RG, Teixeira MJ, Galhardoni R, Silva V, Iglesio R, França C, et al. Connectivity Patterns of Subthalamic Stimulation Influence Pain Outcomes in Parkinson’s Disease. Front Neurol. 2020 Feb 12;11:9.
To cite this abstract in AMA style:
N. Pacheco-Barrios, V. Gagliardi, R. Grudtner, I. Njokanma, K. Acurio, J. Rolston, B. Illigens, F. Fregni, K. Pacheco-Barrios. The Association of Pain with motor symptom severity in Parkinson’s Disease: A secondary data analysis [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/the-association-of-pain-with-motor-symptom-severity-in-parkinsons-disease-a-secondary-data-analysis/. Accessed March 4, 2026.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/the-association-of-pain-with-motor-symptom-severity-in-parkinsons-disease-a-secondary-data-analysis/