Category: Surgical Therapy: Parkinson's Disease
Objective: To describe a rare complication of Deep Brain Stimulation (DBS).
Background: DBS is a surgical treatment for Parkinson´s Disease (PD). Among the possible surgical complications, pneumocephalus (PC) is defined by intracranial air accumulation.
Method: We report a case of a 54-year-old male with a 10-year history of PD. Throughout the years, he developed motor worsening and fluctuations, and impulsivity with high doses of Pramipexol. He was taking Levodopa-Benserazide 1600mg/day and Pramipexol 3mg/day.
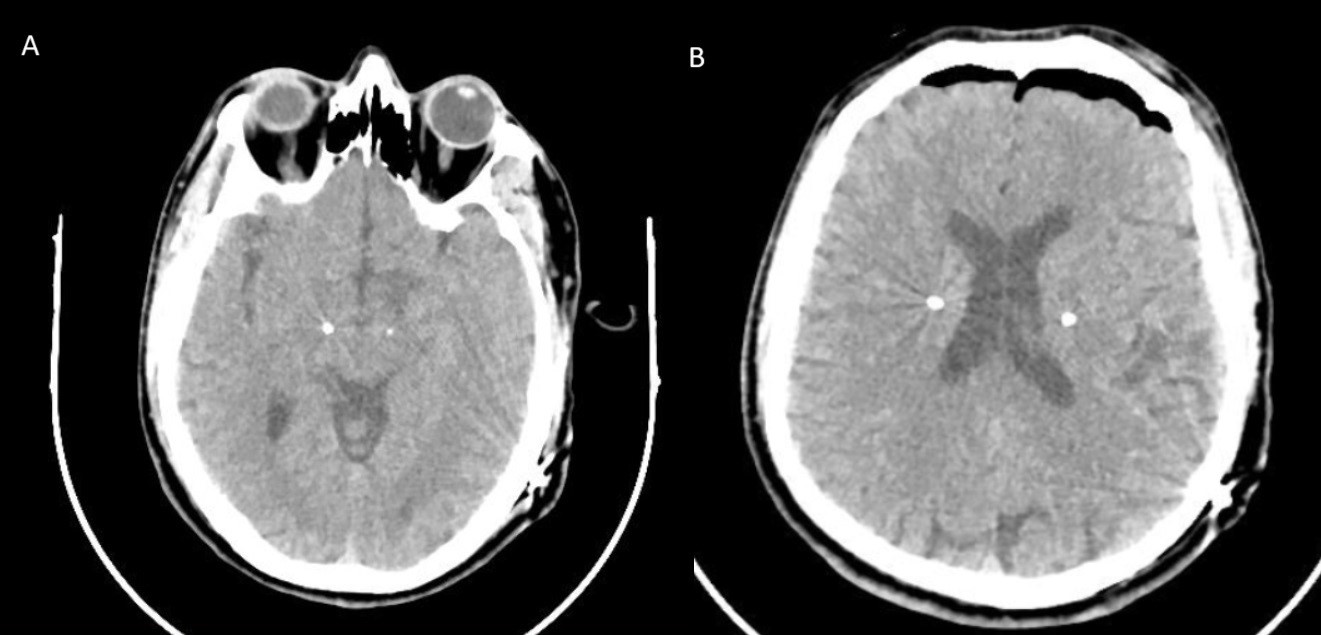
He underwent bilateral Subthalamic Nucleus DBS surgery with good clinical response. The postoperative head Computed Tomography (CT) scan showed well-placed leads and small subdural pneumocephalus (15.5 cm3) (Figure 1).
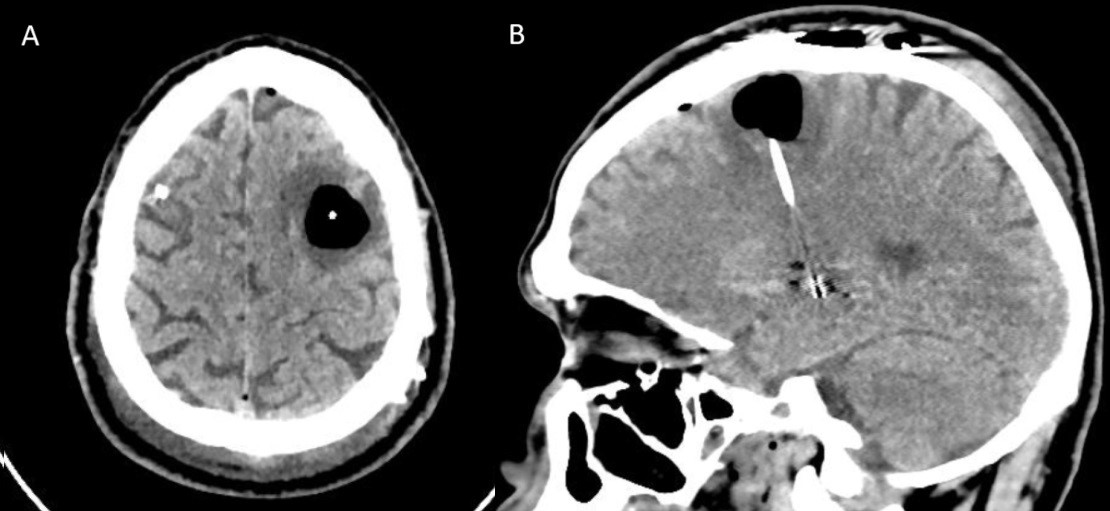
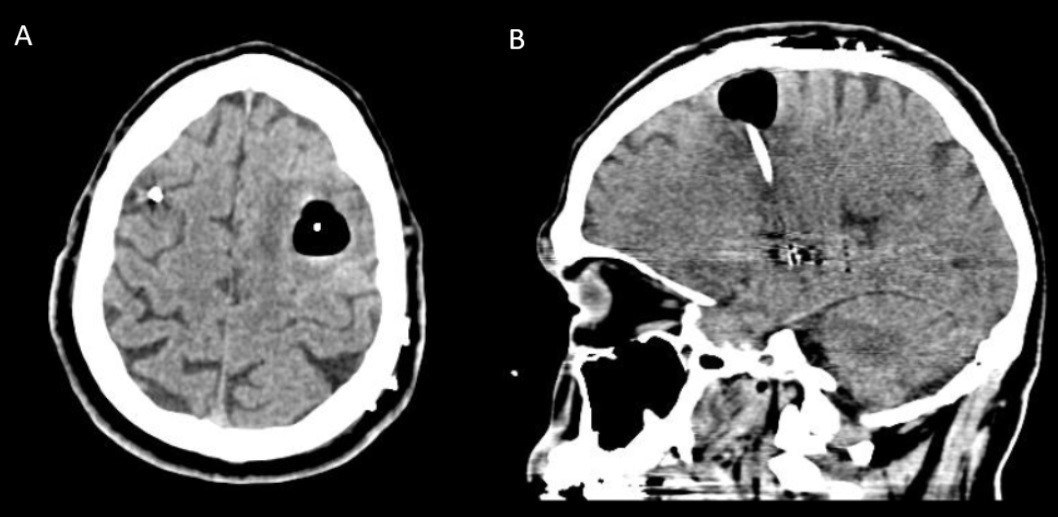
On the 3rd day, he developed mild verbal fluency impairment and right hemiparesis. A new head CT scan showed that PC around the left lead (6.3 cm3) with mild edema (Figure 2). Conservative management was adopted, a new head CT scan (Figure 3) after 2 days showed PC regression (4.8 cm3) and he presented complete clinical recovery.
A literature review on PC was conducted.
Results: PC is commonly seen after craniotomy, although it’s usually asymptomatic and resolves in 2-3 weeks [1]. When it causes brain compression, it’s defined as Tension PC (TPC), mainly seen in posterior fossa or cervical spine surgery in the sitting position [3,4].
Most common PC symptoms include meningism, nausea, altered mental status, seizures, and focal deficits [6]. It’s difficult to clinically differentiate between PC and TPC, although the parenchymal air bubble sign is more likely to occur in TPC [6,7]. While simple PC can be managed conservatively, TPC may require urgent decompressive surgery [8]. In our case, our patient recovered with conservative management.
Two studies showed that mean PC volume is 2.2 (0-87) [9] and 21.5 ± 13.7 cm3 (0-68.8) [10]. Our patient’s postoperative PC volume was within the expected range. Despite PC presenting volume reduction in the following days, air was displaced around the lead and provoked brain compression. Previous reports of symptomatic PC showed that symptoms were associated with increase of intraparenchymal PC volume after 3-5 days, with decrease of subdural and total PC volumes [11].
Conclusion: We presented a case of TPC, a rare complication of DBS surgery. It can be symptomatic after a few days, and it seems to be related to intraparenchymal PC.
Immediate post operative head CT scan.
Head CT scan with TPC and edema, volume of 6.3 cm3
Head CT scan with PC regression, volume of 4.8 cm3
References: 1. Reasoner DK, Todd MM, Scamman FL, Warner DS. The incidence of pneumocephalus after supratentorial craniotomy. Observations on the disappearance of intracranial air. Anesthesiology. 1994 May; 80(5):1008–12.
2. Vanamoorthy P, Tomar A, Prabhakar H, Rath GP. Rare complications during deep brain stimulation surgery for Parkinson’s disease. J Neuroanaesth Crit Care. 2014; 01(02):150–2.
3. Prabhakar H, Bithal PK, Garg A. Tension pneumocephalus after craniotomy in supine position. J Neurosurg Anesthesiol. 2003 Jul; 15(3):278–81.
4. Nazzaro JM, Lyons KE, Honea RA, Mayo MS, Cook-Wiens G, Harsha A, et al. Head positioning and risk of pneumocephalus, air embolism, and hemorrhage during subthalamic deep brain stimulation surgery. Acta Neuro- chir (Wien). 2010 Dec; 152(12):2047–52.
5. Beggio G, Raneri F, Rustemi O, Scerrati A, Zambon G, Piacentino M. Techniques for pneumocephalus and brain shift reduction in DBS surgery: a review of the literature. Neurosurg Rev. 2020; 43(1):95–9.
6. Sweni S, Senthilkumaran S, Balamurugan N, Thirumalaikol-undusubramanian P. Tension pneumocephalus: a case report with review of literature. Emerg Radiol 2013; 20:573-8.
7. Michel SJ. The mount Fuji sign. Radiology. 2004;232(2):449–50.
8. Wankhade BS, Beniamein MMK, Alrais ZF, Mathew JI, Alrais GZ. What should an intensivist know about pneumocephalus and tension pneumocephalus? Acute Crit Care. 2023; 38(2):244–8.
9. Mirzadeh Z, Chen T, Chapple KM, Lambert M, Karis JP, Dhall R, et al. Procedural Variables Influencing Stereotactic Accuracy and Efficiency in Deep Brain Stimulation Surgery. Oper Neurosurg (Hagerstown). 2019 Jul; 17(1): 70–8.
10. Sharim J, Pezeshkian P, DeSalles A, Pouratian N. Effect of cranial window diameter during deep brain stimulation surgery on volume of pneumocephalus. Neuromodulation. 2015 Oct; 18(7): 574–8; discussion 578–9.
11. Albano L, Rohatgi P, Kashanian A, Bari A, Pouratian N. Symptomatic Pneumocephalus after Deep Brain Stimulation Surgery: Report of 2 Cases. Stereotact Funct Neurosurg. 2020;98(1):30-36. doi: 10.1159/000505078. Epub 2020 Feb 4. PMID: 32018273.
To cite this abstract in AMA style:
E. Rosa Fernandes, L. Bassani Devens, G. Dick Bonato, J. Junqueira Bizzi, L. Frighetto, P. Petry Oppitz, S. Trentin, B. Fraiman Oliveira, Y. Felloni Borges. Tension Pneumocephalus as an acute complication of STN-DBS surgery [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/tension-pneumocephalus-as-an-acute-complication-of-stn-dbs-surgery/. Accessed December 23, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/tension-pneumocephalus-as-an-acute-complication-of-stn-dbs-surgery/