Session Information
Date: Monday, October 8, 2018
Session Title: Parkinson's Disease: Non-Motor Symptoms
Session Time: 1:15pm-2:45pm
Location: Hall 3FG
Objective: To assess the relationship between subjective and objective urinary dysfunction in patients with Parkinson’s disease (PD), multiple system atrophy (MSA), and progressive supranuclear palsy (PSP), and to determine the correlation between clinical characteristics and subjective urinary dysfunction or post-void residual urine volume.
Background: In clinical practice urinary dysfunction is generally assessed by subjective urinary dysfunction questionnaires and sonographic post-void residual urine volumes. However, subjective urinary dysfunctions are weakly correlated with objective tests.
Methods: A total of 196 de novo patients with PD, MSA, and PSP without urological and gynecological disorders were enrolled using each clinical diagnostic criterion. Data were collected on sonographic post-void residual urine volumes and urinary symptoms using questionnaires. All patients were also assessed with motor symptoms, cognitive measurements, other non-motor symptoms, and renal functions.
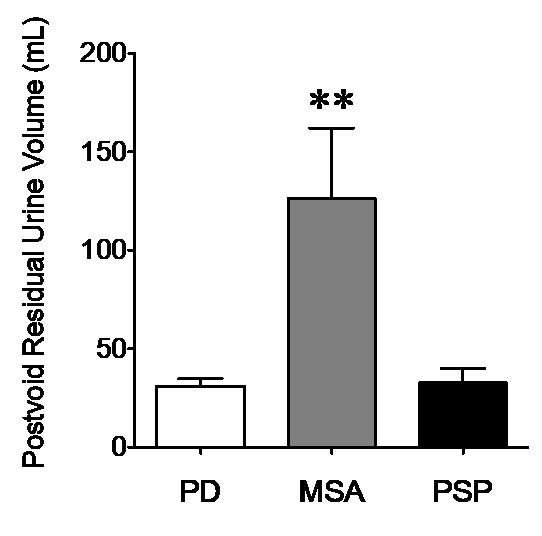
Results: Abnormal post-void residual urine volume was found in 10 out of 163 PD patients, 6 out of 14 MSA patients, and 1 out of 19 PSP patients. The MSA group showed significantly higher post-void residual urine volume compared to the PD and PSP groups. Symptoms of the sense of incomplete emptying, weak urine stream, and nocturia were strongly correlated with post-void residual urine volume. Post-void residual urine volume was positively related to autonomic symptoms, other non-motor symptoms, patient activities of daily living, and negatively related to renal function.
Conclusions: In conclusion, significantly increased sonographic post-void residual urine volumes were observed in a small portion of early de-novo drug naive Parkinsonian patients, especially in MSA patients. Objectively measured post-void residual urine volume was significantly related to subjective urinary dysfunctions and other autonomic dysfunctions. Therefore, voiding problems due to urinary dysfunction requires attention and investigation of urinary dysfunction in PD patients.
References: [1] Fragal`a E, Russo GI, Di Rosa A, Giardina R, Privitera S, Favilla V, Patti F, Welk B, Cimino S, Castelli T, Morgia G (2015) Association between the neurogenic bladder symptom score and urodynamic examination in multiple sclerosis patients with lower urinary tract dysfunction.Int Neurourol J 19, 272-277. [2] Badri AV, Purohit RS, Skenazy J, Weiss JP, Blaivas JG (2014) A review of lower urinary tract symptoms in patients with Parkinson’s disease. Curr Urol Rep 15, 435.
To cite this abstract in AMA style:
Y. Lee, J. Kim. Subjective and objective urinary dysfunction in parkinson’s disease and atypical parkinsonisms [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/subjective-and-objective-urinary-dysfunction-in-parkinsons-disease-and-atypical-parkinsonisms/. Accessed January 1, 2026.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/subjective-and-objective-urinary-dysfunction-in-parkinsons-disease-and-atypical-parkinsonisms/