Category: Parkinson's Disease: Neuroimaging
Objective: To evaluate the relationship between various measures of subcortical atrophy with fall risk in PD.
Background: Falls occur in nearly 70% of people with idiopathic Parkinson’s disease [1]. Imaging studies have correlated reduced gray matter, decreased thalamic cholinergic activity, and larger ventricular volumes with greater risk of falls in patients with PD [2] [3] [4]. We hypothesize that fall risk correlates with easily acquirable measures of subcortical atrophy in people with PD.
Method: This pilot study is a retrospective chart review that investigated demographic information, PD subtype, and subcortical atrophy measures from recent (up to 1 year) imaging findings. Subcortical atrophy measures used in this study included bicaudate ratio (BCR), Evan’s Index (EI), and third ventricular width (TVW). Each participant was then administered a standardized and validated fall risk questionnaire (FRQ).
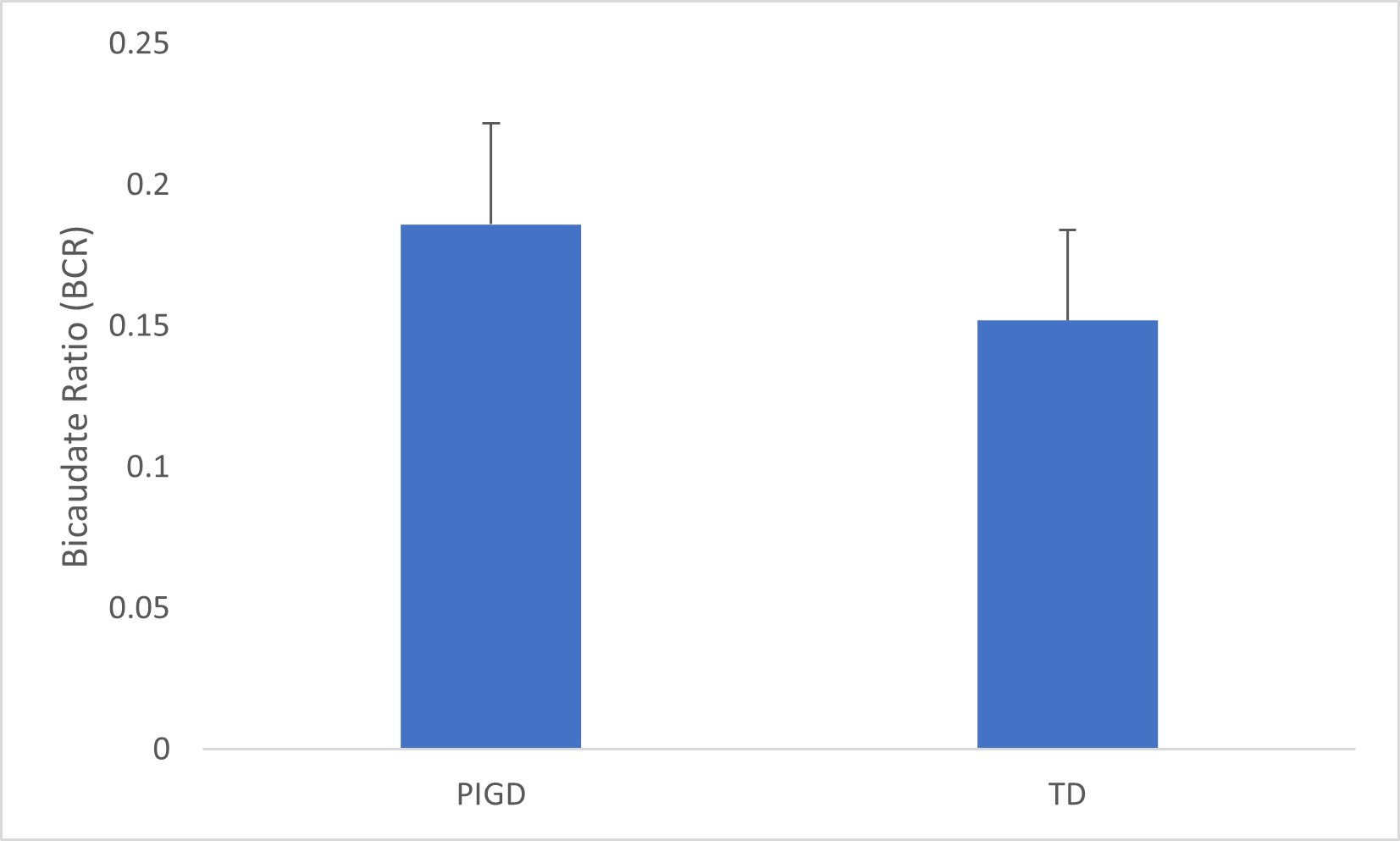
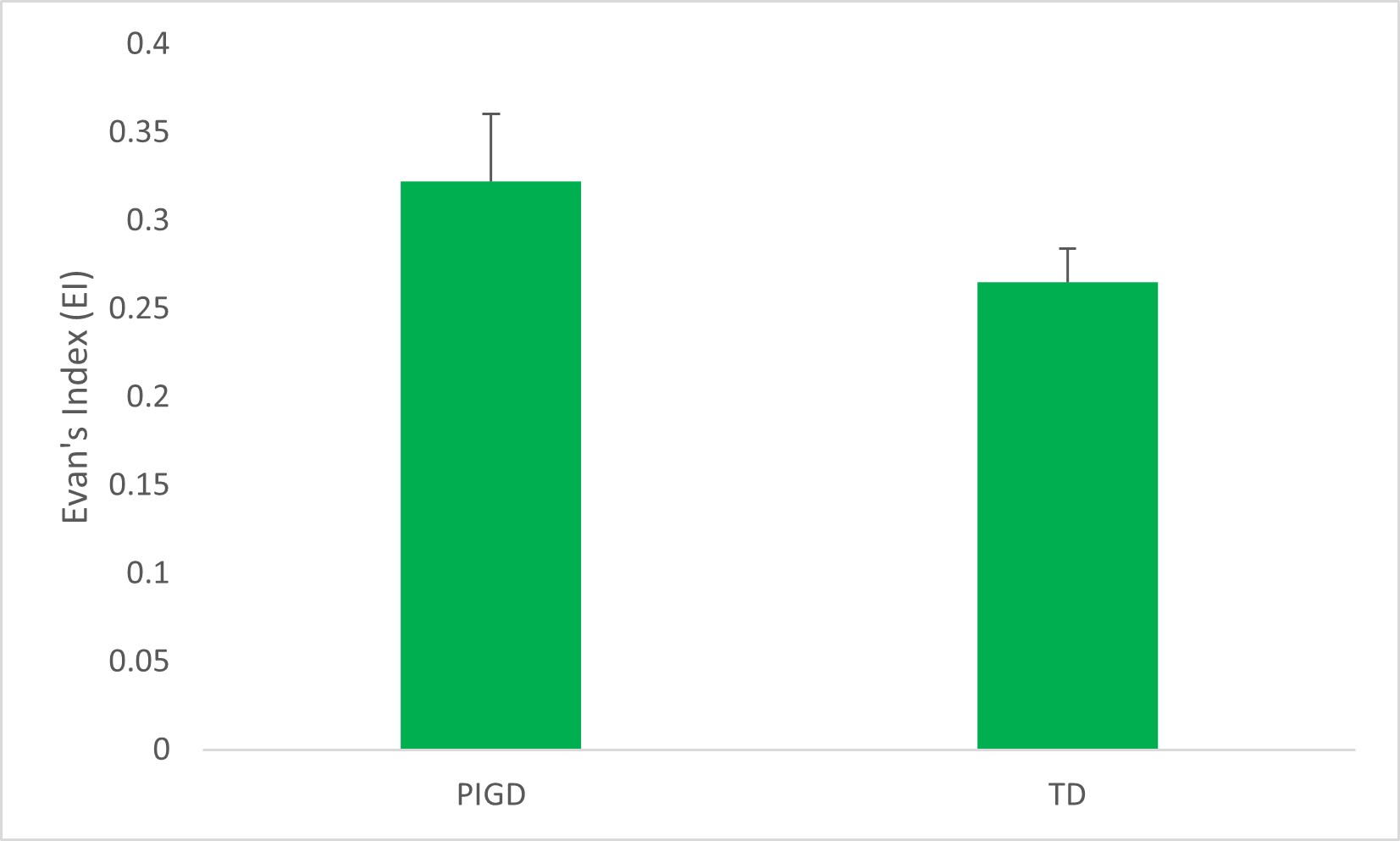
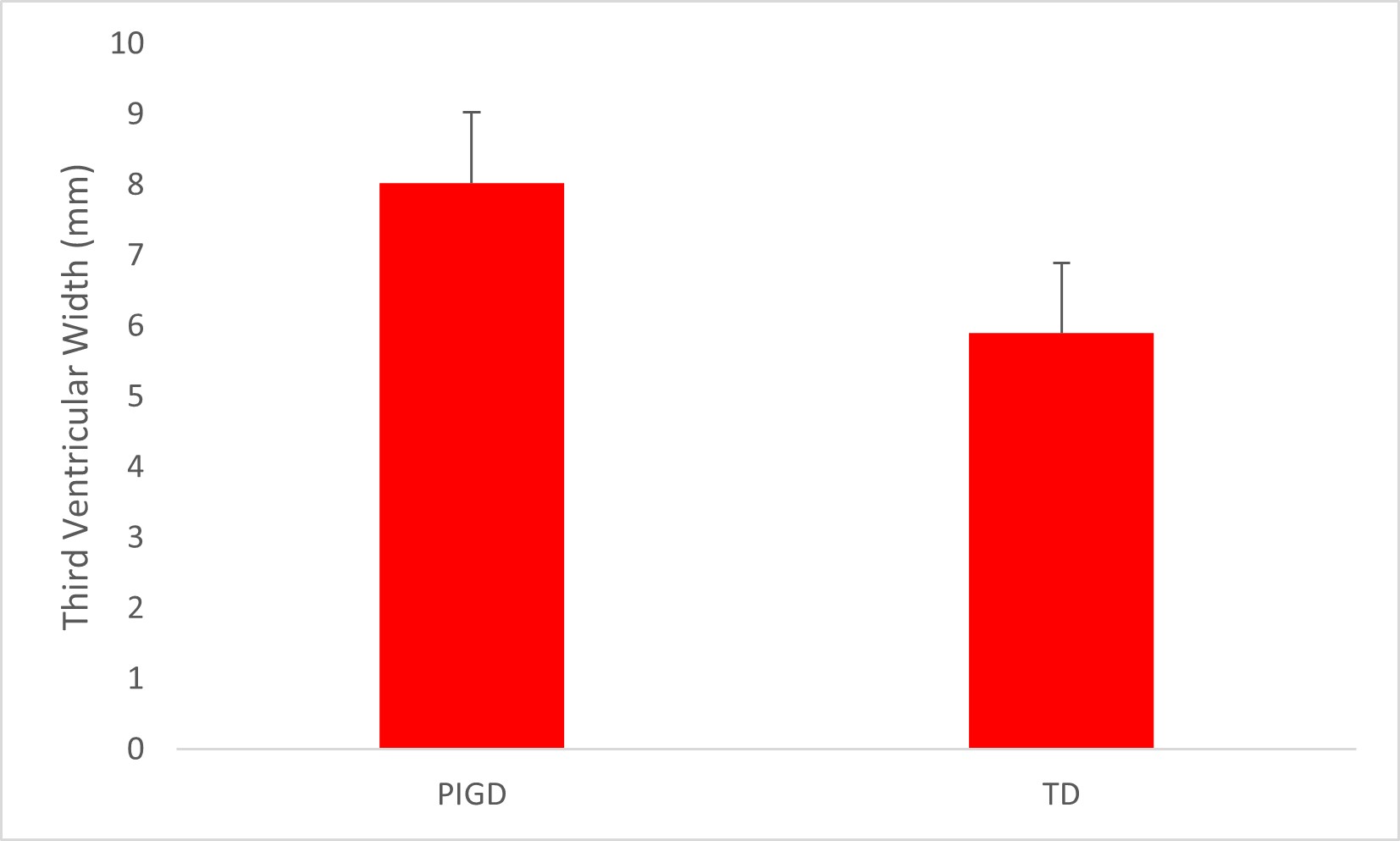
Results: From the 17 patients analyzed, 5 patients had postural-instability-gait-disturbance predominant PD (PIGD) and 10 had tremor predominant PD (TD), where 2 had a mixed subtype. PIGD patients had lower mean scores for bicaudate ratio (BCR), Evan ventricular index (EI), and third ventricular width (TVW). Mean difference between TD and PIGD was 0.03, 0.06, and 2.34 for the BCR, EI, TVW, respectively. Only EI and TVW demonstrated statistical significance in their differences between the 2 subtypes on Student’s t test (p < 0.05). None of the measures correlated with fall risk as obtained by the FRQ.
Conclusion: Allowing for limitations within this pilot study, people with PIGD subtype PD have on average, more subcortical atrophy than patients with TD subtype PD as measured by Evan’s Index and third ventricular width, but not bicaudate ratio. Future directions for this study include incorporating a larger sample size and employing subgroup analysis on subcortical atrophy and fall risk in the different PD subtypes in relation to the FRQ.
References: 1. Wood B, Bilclough J, Bowron A, Walker R. 2002. Incidence and prediction of falls in Parkinson’s disease: a prospective multidisciplinary study. Journal of Neurology, Neurosurgery, and Psychiatry, 72:721-5.
2. Acharya H, Bouchard T, Emery D, Camicioli R. 2007. Axial signs and magnetic resonance imaging correlates in Parkinson’s disease. The Canadian Journal of Neurological Sciences, 34(1):56-61.
3. Bohnen N, Muller M, Koeppe R, Studenski S, Kilbourn M, Frey K, Albin R. 2009. History of falls in Parkinson disease is associated with reduced cholinergic activity. Neurology, 73(2):1670-6.
4. Rosenberg-Katz K, Herman T, Jacob Y, Giladi N, Hendler T, Hausdorff J. 2013. Gray matter atrophy distinguishes between Parkinson disease motor subtypes. Neurology, 80(16):1476-84.
To cite this abstract in AMA style:
S. Aggarwal, J. Ma, M. Salgado, M. Hamed. Subcortical Atrophy and Fall Risk in Parkinson’s Disease [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/subcortical-atrophy-and-fall-risk-in-parkinsons-disease/. Accessed December 24, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/subcortical-atrophy-and-fall-risk-in-parkinsons-disease/