Session Information
Date: Thursday, June 8, 2017
Session Title: Parkinson's Disease: Neuroimaging And Neurophysiology
Session Time: 1:15pm-2:45pm
Location: Exhibit Hall C
Objective: Using the Progressive Parkinson’s Initiative (PPMI) data, clinical and structural differences between individuals destined to develop PD cognitive impairment was defined.
Background: Cognitive dysfunction in PD is often associated with disease progression. However, subtle deficits can be detected in 24% of individuals at diagnosis1, suggesting that damage is already present.
Methods: COHORT SELECTION:
Individuals with PD and a 3T T1-weighted MRI at baseline were selected and divided into three groups based on their eventual cognitive status: No dementia (PD-NON, N=207), mild cognitive impairment (PD-MCI, N=102), or dementia (PDD, N=9).
IMAGE PRE-PROCESSING:
The T1 weighted MRI was segmented into grey matter (GM) and white matter (WM) using SPM12 and used for voxel-based morphometry (VBM), applying a 6mm FWHM Gaussian smoothing kernel.
IMAGE ANALYSIS
Structural differences were tested using a one-way ANOVA in SPM12, controlling for age, gender, handedness, years of education, TIV and study center. Significance was set at peak voxel Family Wise Error (FWE) P < 0.05.
CLINICAL DATA
Group differences were assessed using a Kruskal-Wallis test.
Results: CLINICAL
The PD-MCI and PDD groups were significantly older with more severe motor and non-motor symptoms (anosmia, RBD and depression).
VBM:GM
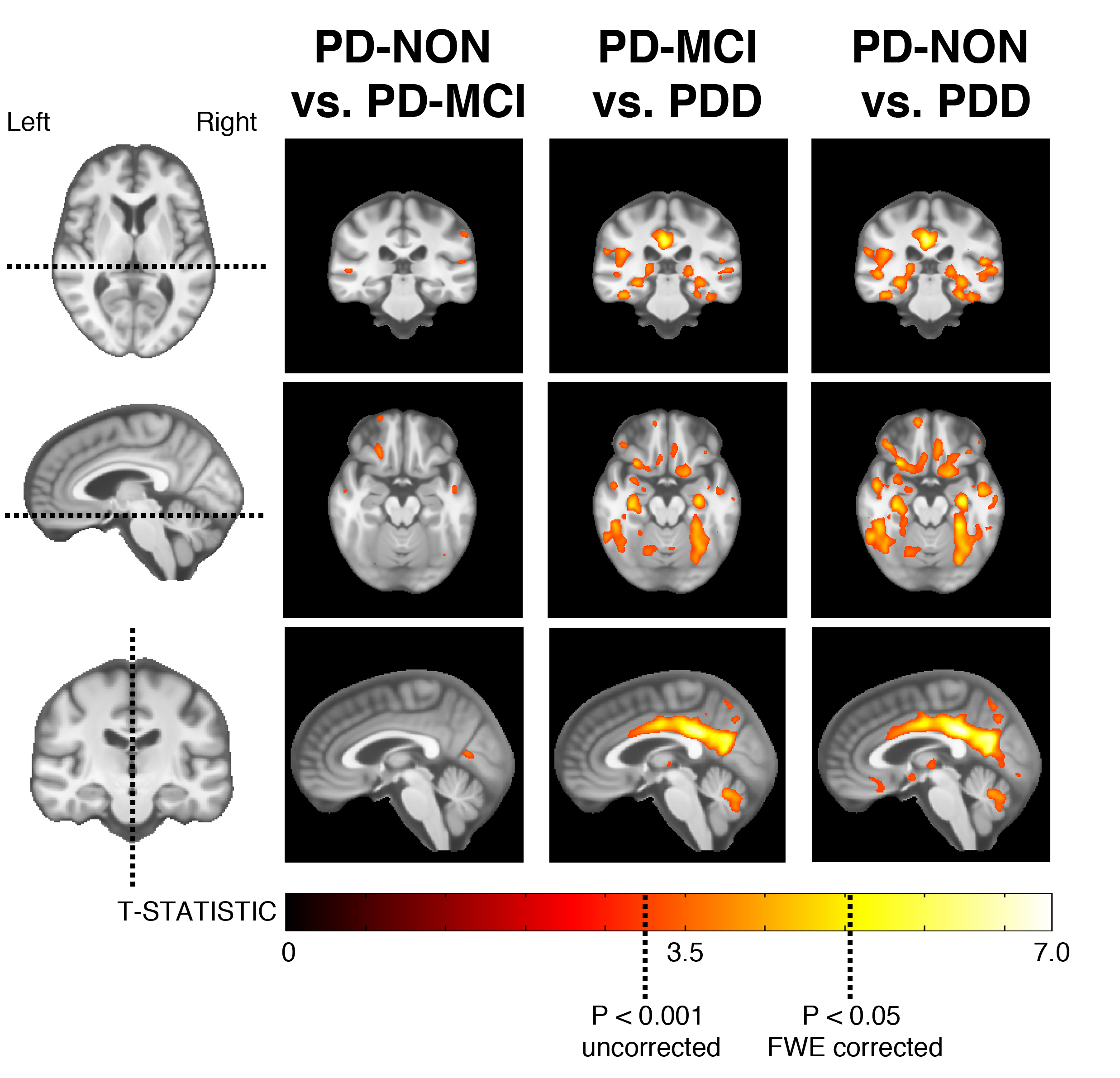
Widespread areas of reduced GM were observed between PD-NON vs. PDD and PD-MCI vs. PDD, particularly in the bilateral hippocampi, primary olfactory cortex, posterior cingulate and cerebellum. Fewer abnormalities were observed between PD-NON vs. PD-MCI, and included the temporal-parietal junction and cerebellum (Figure 1).
[figure1]
VBM:WM
Several areas of reduced WM were observed between PD-NON vs. PDD and PD-MCI vs. PDD, particularly in the parietal WM.
Conclusions: 1. There are no significant differences surviving multiple comparison correction in the baseline cognitive profile or disease duration between the three groups.
2. Those who develop PD-MCI or PDD are significantly older with more severe motor and non-motor symptoms (anosmia, RBD and depression).
3. The average time to MCI is no different between the PD-MCI and PDD groups.
4. Extensive grey and white matter loss is present at least three years before dementia clinically manifests in PD.
5. Abnormalities in pre-clinical PD-MCI overlap with preclinical PDD, suggesting an intermediate stage.
References: 1. Muslimović, D., Post, B., Speelman, J.D. and Schmand, B., 2005. Cognitive profile of patients with newly diagnosed Parkinson disease. Neurology, 65(8), pp.1239-1245.
To cite this abstract in AMA style:
C. Lambert, O. Williams, L. Ricciardi, F. Morgante, T. Barrick, M. Edwards. Structural brain abnormalities associated with preclinical cognitive impairment in Idiopathic Parkinson’s Disease. [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/structural-brain-abnormalities-associated-with-preclinical-cognitive-impairment-in-idiopathic-parkinsons-disease/. Accessed January 18, 2026.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/structural-brain-abnormalities-associated-with-preclinical-cognitive-impairment-in-idiopathic-parkinsons-disease/