Category: Other
Objective: To present an unusual presentation of paraneoplastic stiff-person syndrome (SPS).
Background: SPS may have paraneoplastic, autoimmune, or cryptogenic etiology and most often be associated with anti-GAD65-IgG and anti-amphiphysine-IgG.
Method: Case report.
Results: A 40-year-old woman presented to our clinic with stiffness and involuntary spasms in the lower extremities. These symptoms appeared 13 months ago, at the same time she was diagnosed with a low-grade ovarian carcinoma with metastases to the peritoneum and lymph nodes. After the full cytoreduction and chemotherapy (paclitaxel+carboplatin) cancer remission was achieved, however neurological symptoms kept progressing.
On admission her neurological examination revealed no abnormalities with her mental status, cranial nerves. She demonstrated severe stiffness in the lower extremities, axial rigidity, painful spasms triggered by position changing or tactile stimulus. Her legs, knees and toes were in extension. No signs of ataxia were noted. She was ambulating with walker assistance.
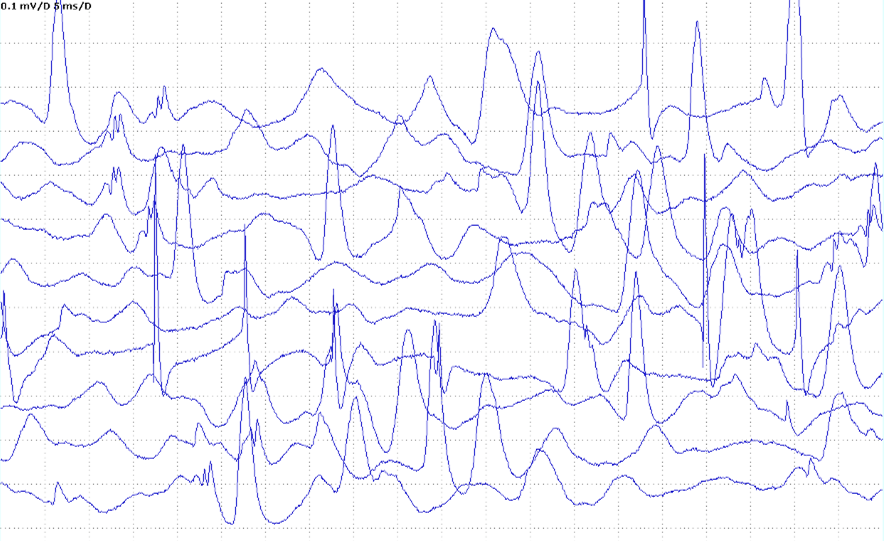
Brain and spinal MRI, EEG didn’t find any abnormalities. EMG showed discharging motor unit potential in m. paravertebralis Th12, m. vastus lateralis and m. tibialis [figure1]. Serum was positive for anti-Yo1-IgG and negative for other antineuronal antibodies (include anti-amphiphysin-IgG, anti-GAD65-IgG). CSF exams showed no pleocytosis, no oligoclonal bands, no anti-GAD65-IgG. Indirect immunofluorescence assay of antineuronal antibodies in CSF was positive (1:4, Purkinje cell luminescence). There were no signs of cancer relapse on serum CA-125, 18F-FDG PET-CT, pelvic MRI.
She was treated with a PLEX, IVMP, diazepam 50 mg/day with the following symptoms improvement. Even though painful spasms completely resolved, muscle stiffness and axial rigidity persisted, so IVIG (2 g/kg at month) was planned.
Conclusion: This case of paraneoplastic SPS is unusual due to neurological symptoms deterioration after the cancer treatment. Moreover, the association of SPS with anti-Yo1 isn’t typical. The absence of ataxia in anti-Yo-1 disorder is also unusual (although subclinical cerebellar dysfunction cannot be excluded). However, our patient’s disease corresponded to the clinical and EMG diagnostic criteria of SPS.
To cite this abstract in AMA style:
E. Chekanova, I. Luneva, A. Kozlova, O. Smetanina, M. Zakharova. Stiff-person syndrome associated with anti-Yo1 antibodies: a case report [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/stiff-person-syndrome-associated-with-anti-yo1-antibodies-a-case-report/. Accessed April 17, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/stiff-person-syndrome-associated-with-anti-yo1-antibodies-a-case-report/