Session Information
Date: Tuesday, June 6, 2017
Session Title: Huntington's Disease
Session Time: 1:45pm-3:15pm
Location: Exhibit Hall C
Objective: The need to differentiate the malingering from real complains
Careful history can give a strong clue for the diagnosis
Criminals can have diseases also
Background: It is common that the physician can be affected by the patient’s background. Malingering is a well-known entity but we should be extremely careful when diagnosing such a case in a patient presenting with complicated symptoms, regardless if he is a criminal or not.
Methods: we are presenting a case of a patient , who is a prisoner presented with abnormal movements. The patient is a 37y old smuggler, presented with abnormal movements since age 31y. The patient was seen at that time by a medical committee to decide if he is fit to stay at prison. In view of the recent onset of the patient symptoms, negative family history and lake of hard evidence of neurological disease, he was diagnosed as malingering and send back to jail.
On 2016, the patient was brought again with progression of his symptoms. In addition, he has dysartheria, dysphagia and weight loss progressive for the last 1 year. The patient also mentioned that he has a younger brother who started to have similar symptoms. The patient was examined and found to have deteriorated mental function, dysartheria, dysphagia, bilateral abnormal asymmetric, involuntary movements affecting the face especially the lips and tongue in addition to distal limbs. The rest of the neurological exam was normal.
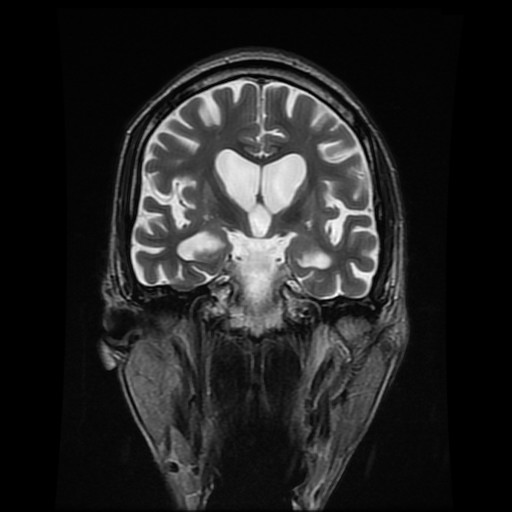
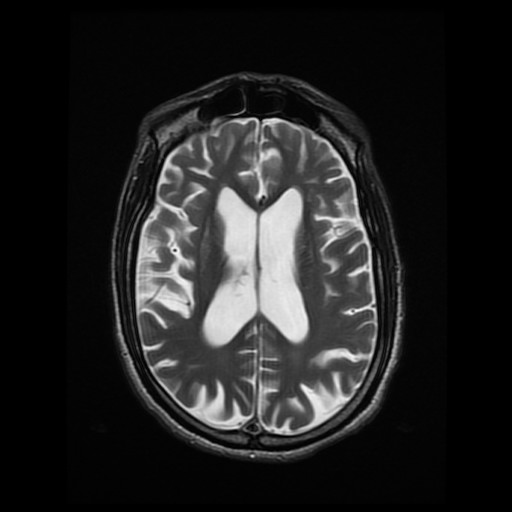
Results: The patient had MRI brain, which showed general brain atrophy and sever atrophic changes in the basal ganglia especially the head of the caudate nucleus. Huntington disease was suspected and the genetic testing was ordered. Meanwhile, the liver function tests, copper, ceruloplasmin and 24h urine copper all came negative. The result of the genetic test came positive with CAG triplet of 46 on one of the alleles.
Conclusions: The real epidemiology of Huntington’s disease is not known. It should be suspected in any young onset abnormal movement of choreic forms. Malingering should be the last diagnosis to consider even in a prisoner.
References: Corrêa BB, Xavier M, Guimarães J. Association of Huntington’s disease and schizophrenia-like psychosis in a Huntington’s disease pedigree. Clinical Practice and Epidemiology in Mental Health : CP & EMH. 2006;2:1. doi:10.1186/1745-0179-2-1. Jardri R, Medjkane F, Cuisset JM, Vallee L, Delion P, Goeb JL.Huntington’s disease presenting as a depressive disorder with psychotic features. J Am Acad Child Adolesc Psychiatry 2007;46:307-308. Fistikci N, Saatcioglu O, Erten E, Yilmaz G, Calci C, Keyvan A. Treatment resistant obsessive compulsive disorder and psychosis due to Huntington’s disease. Marmara Medical Journal 2013; 26:105-107
To cite this abstract in AMA style:
A. Alboudi, P. Sarathchandran, A.B. Almadani. Social hindrances for diagnosing Huntington’s disease [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/social-hindrances-for-diagnosing-huntingtons-disease/. Accessed December 22, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/social-hindrances-for-diagnosing-huntingtons-disease/