Session Information
Date: Monday, September 23, 2019
Session Title: Quality of Life
Session Time: 1:45pm-3:15pm
Location: Les Muses Terrace, Level 3
Objective: To determine correlates of nocturnal sleep dysfunction in patients with idiopathic Parkinson’s disease (PD).
Background: Nocturnal sleep disturbances are among the most prevalent non-motor symptoms of PD. Although they have been associated with disease duration[1] and severity[2], cognitive impairment[3, 4], and even complications of treatment like dyskinesias[5]; their impact on patient’s quality of life remains understudied.
Method: Retrospective analytical study. Case files of PD patients were reviewed, and those with complete Parkinson’s Disease Sleep Scale (PDSS) scores were included for analysis. Bivariate correlations were determined between PDSS total score and subscores and Quality of Life score (8-item PD Questionnaire, PDQ8), Hoehn & Yahr stage, motor (MDS-UPDRS III), and cognitive (MoCA) scores.
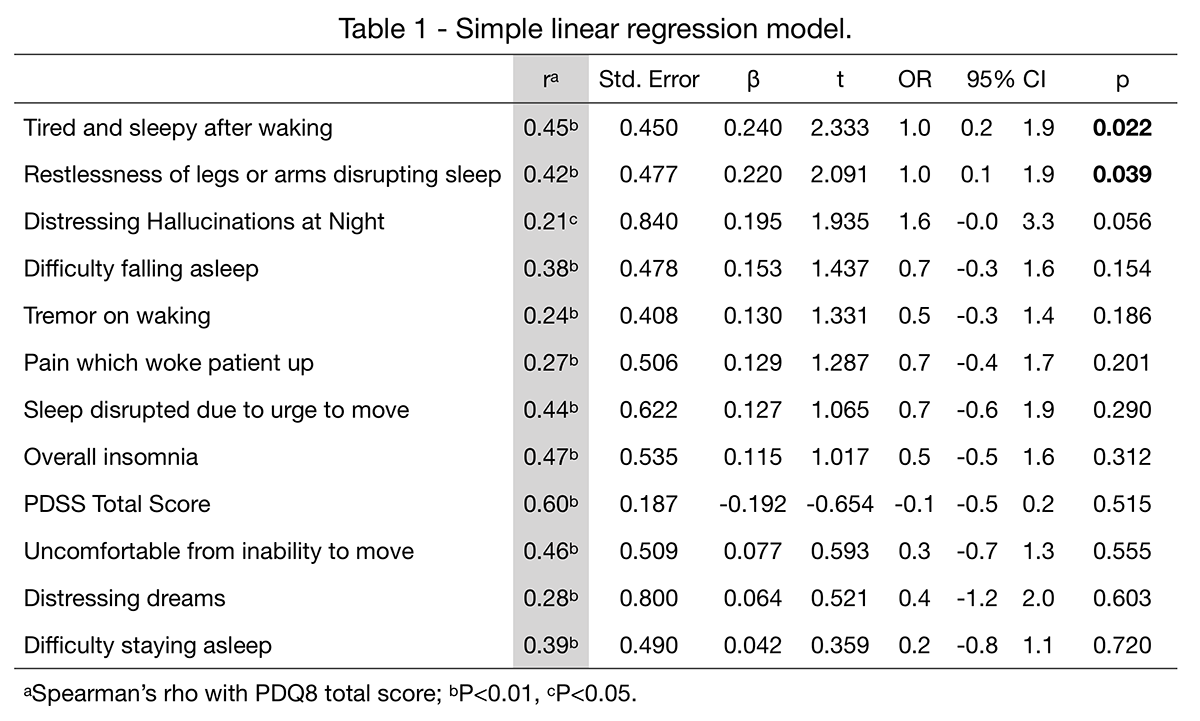
Results: 105 cases were analyzed, 68% male (n=71), mean age 60.2±11.9, age at onset 54.7±12.8 and disease duration 6.8±5.5 years. Mean Hoehn & Yahr 2.4±0.9, MDS-UPDRS III 41.7±25.3, and MoCA 24.0±4.2. Mean PDSS score was 15.7±10.1; the most frequent disturbance was nocturia (n=77, 73%), followed by inability to move (n=59, 56%), and morning tiredness (n=56, 53%). Mean PDQ8 score was 9.6±6.4, and the most frequent domains impaired were ‘difficulty dressing’ (n=73, 70%), ‘feeling depressed’ (n=70, 67%), and ‘painful muscle cramps’ (n=69, 66%). We found positive correlations between PDQ8 and total PDSS score (r=0.60, p<0.01) and subscores ‘tiredness upon waking’ (r=0.45, p<0.01), and ‘limb-restlessness disrupting sleep’ (r=0.42, p<0.01). A linear regression model with PDQ8 total score as dependent variable, and PDSS subscores as predictors showed that ‘tiredness upon waking’ (OR 1.0, 95%CI 0.2–1.9) and ‘limb-restlessness disrupting sleep’ (OR 1.0, 95%CI 0.1–1.9) were the only statistically significant predictors (p=0.02 and p=0.04 respectively) of quality of life (Table 1).
Conclusion: Although the most frequently reported disturbance of sleep is nocturia, and patient-reported experiences of daily life (both motor and non-motor) and quality of life scores are correlated with nocturnal sleep disturbances, only limb restlessness that disrupts sleep represents a statistically significant predictor of quality of life.
References: 1. Bjornara KA, Dietrichs E, Toft M. Clinical features associated with sleep disturbances in Parkinson’s disease. Clin Neurol Neurosurg. 2014;124:37-43. 2. Junho BT, Kummer A, Cardoso FE, Teixeira AL, Rocha NP. Sleep quality is associated with the severity of clinical symptoms in Parkinson’s disease. Acta Neurol Belg. 2018;118(1):85-91. 3. Goldman JG, Ghode RA, Ouyang B, Bernard B, Goetz CG, Stebbins GT. Dissociations among daytime sleepiness, nighttime sleep, and cognitive status in Parkinson’s disease. Parkinsonism Relat Disord. 2013;19(9):806-11. 4. Goldman JG, Stebbins GT, Leung V, Tilley BC, Goetz CG. Relationships among cognitive impairment, sleep, and fatigue in Parkinson’s disease using the MDS-UPDRS. Parkinsonism Relat Disord. 2014;20(11):1135-9. 5. Mao CJ, Yang YP, Chen JP, Wang F, Chen J, Zhang JR, et al. Poor nighttime sleep is positively associated with dyskinesia in Parkinson’s disease patients. Parkinsonism Relat Disord. 2018;48:68-73.
To cite this abstract in AMA style:
D. Martínez-Roque, S. Castillo-Torres, C. Cerda-Contreras, I. Estrada-Bellmann, B. Chávez-Luévanos. Sleep-related quality of life predictors in Parkinson’s disease [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/sleep-related-quality-of-life-predictors-in-parkinsons-disease/. Accessed December 13, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/sleep-related-quality-of-life-predictors-in-parkinsons-disease/