Category: Parkinson's Disease: Non-Motor Symptoms
Objective: Assess the feasibility of systematic depression screening of people with Parkinson’s (PWP) and determine barriers in the specialist movement disorders setting.
Background: While depression is commonly experienced among PWP, depression screening practices for the majority of PWP are inconsistent. Within Parkinson’s Foundation Centers of Excellence (PF COE), a substantial proportion of PWP (> 50%) with identifiable symptoms of depressed mood are not receiving pharmacologic intervention or mental health services. Systematic depression screening could not only identify untreated depression in PWP but also allows monitoring of treatment response, ultimately improving quality of life.
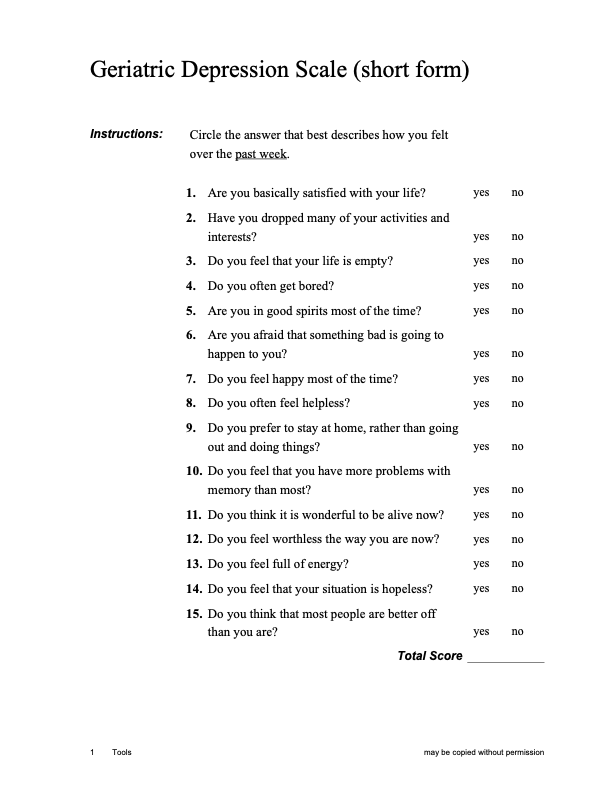
Method: Systematic depression screening of PWP attending appointments for follow-up care is being implemented at 5 PF COE sites using the 15-item Geriatric Depression Scale (GDS-15). To understand pre-existing depression screening practices, diagnosis and treatment practices, 10 patient medical records per clinician at each site will be reviewed. Qualitative interviews with clinicians and PWP will be conducted to understand feasibility and barriers to implementation. Depression-specific educational resources and a treatment algorithm are being provided to the health care team. Up to 130 PWP who screen positive for depression (GDS-15 > 4) will be invited to a prospective study of 12 months that will collect PDQ-39, GDS-15 and depression treatment data.
Results: Primary outcome measures are the proportion of PWP that complete the GDS-15 at clinical visits and the feasibility of incorporating systematic screening into routine care. Secondary outcome measures include: 1) the difference in the proportion of PWP screened for depression in the one-year period before and during the study period; 2) the proportion of responders to depression care among those screening positive , where a reduction in GDS-15 score of 50% between baseline and 12 months is considered a response; and 3) the change in PDQ-39 emotional subscales between baseline and the follow-up visits up to 12-months among those screening positive for depression.
Conclusion: Implementation of systematic depression screening in PWP will improve the standard of care for PD by raising awareness among both clinicians and PWP and by providing treatment decision aides to improve quality of life.
To cite this abstract in AMA style:
Z. Meyer, C. Marras, A. Naito, N. Dahodwala, A. Ramirez-Zamora, M. Rose Rafferty, M. Neault, J. Beck, R. Deleon, T. Davis, S. Mantri, K. Mills, J. Miyasaki, E. Nelson, A. Brown, D. Weintraub, A. Allen. Screening and Treatment of Depression in Parkinson’s Disease within Movement Disorders Centers: A Quality Improvement Initiative [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/screening-and-treatment-of-depression-in-parkinsons-disease-within-movement-disorders-centers-a-quality-improvement-initiative/. Accessed April 26, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/screening-and-treatment-of-depression-in-parkinsons-disease-within-movement-disorders-centers-a-quality-improvement-initiative/