Session Information
Date: Wednesday, September 25, 2019
Session Title: Non-Motor Symptoms
Session Time: 1:15pm-2:45pm
Location: Agora 3 West, Level 3
Objective: To investigate the relationship between pain and autonomic symptoms in Parkinson’s disease.
Background: Pain is a relevant non-motor symptom (NMS) affecting the quality of life of patients with Parkinson’s disease (PD)[1], however the precise pathophysiological mechanisms that drives painful symptoms are not yet fully understood. Autonomic symptoms are also common in parkinsonian patients [2] and often cluster with pain, possibly implicating a common pathophysiology.
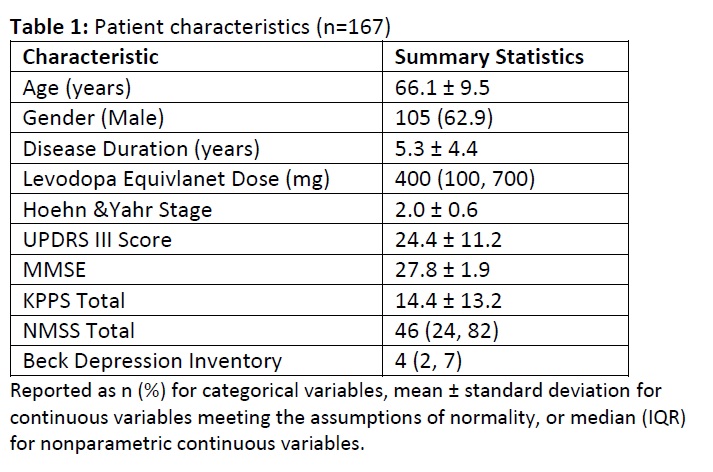
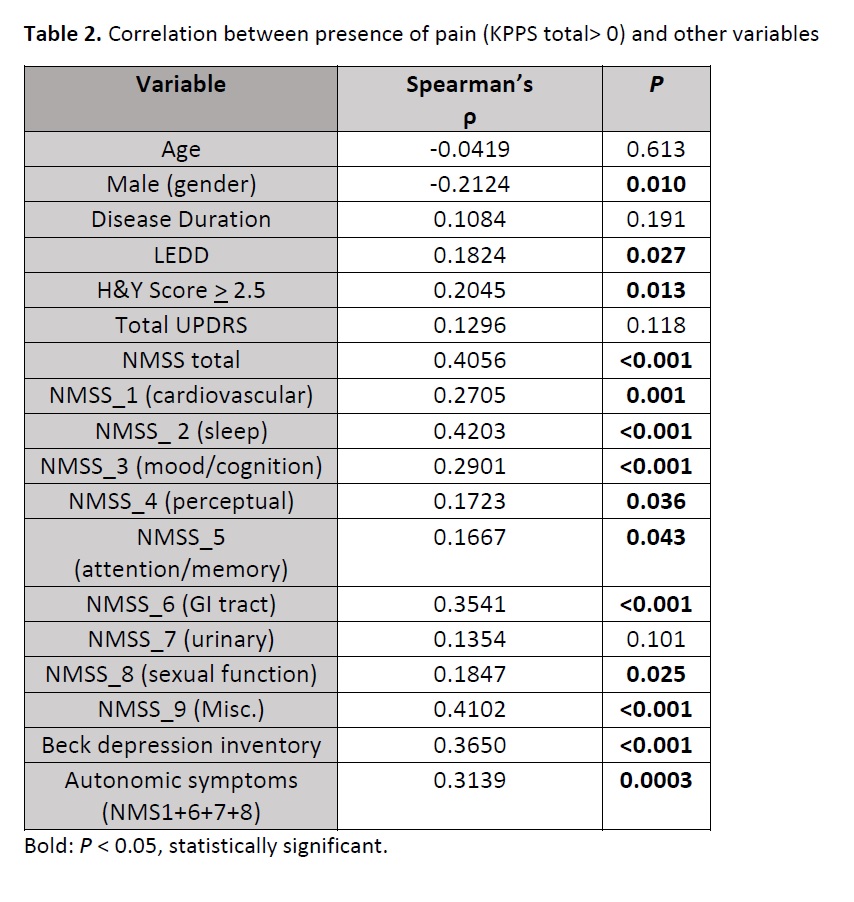
Method: We conducted a cross-sectional observational study on 167 patients with idiopathic PD. Subjects were assessed with UPDRS-part III, H&Y stage, King’s Parkinson’s Disease Pain Scale (KPPS)[3], Non Motor Symptoms Scale (NMSS) and Beck Depression Inventory (BDI). Exclusion criteria were atypical Parkinsonism, cognitive impairment (MMSE≤24/30), severe disability (H&Y stage≥4), or other diseases causing acute or chronic pain. Spearman’s rank correlation coefficient and multiple regression were used for data analysis.
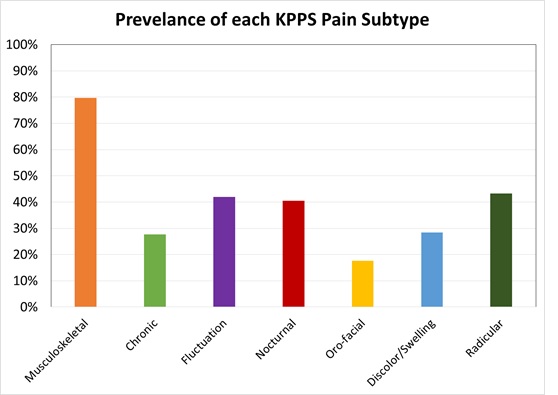
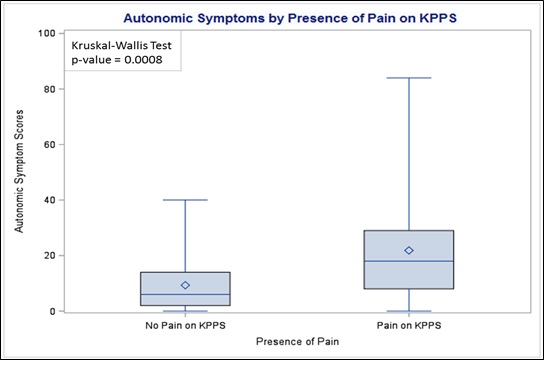
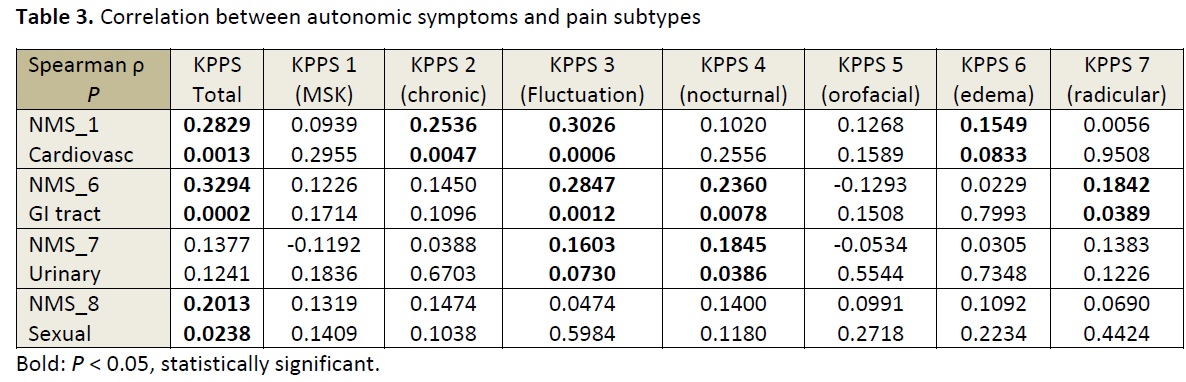
Results: Table 1 summarizes the characteristics of the study population [Table 1]. The prevalence of pain (defined as KPPS total > 0) was 88.6%, in line with previous studies [4] [Figure 1]. Pain correlated with multiple NMS [Table 2]. Multiple regression analysis (F=19.95; P<0.001) with R2=0.42 revealed independent associations between pain and female gender (P=0.003), cardiovascular disturbance (P=0.001) and sleep disruption (P<0.001). Dysautonomia, depression and sleep disturbance each had the strongest correlations with pain. Dysautonomia score was evaluated considering NMSS domain 1 (cardiovascular), 6 (gastrointestinal), 7 (urinary) and 8 (sexual dysfunction). Patients with pain had significantly higher autonomic symptoms scores than patients without pain (P=0.0008) [Figure 2]. Among autonomic symptoms, cardiovascular and gastrointestinal disturbances had the strongest correlation with pain and correlated across multiple pain subtypes [Table 3].
Conclusion: Pain is a frequent symptom in PD. Our analysis shows a possible link between pain and dysautonomia, suggesting a common pathophysiology. We hypothesize a shared pathophysiology of degeneration in brainstem monoamine pathways from early stages of PD, which underpins autonomic symptoms and altered processing of pain [5]. Further studies are warranted to better comprehend the pathogenesis of pain in PD, and for specific potential treatments.
References: [1] Storch A et al (2013). Neurology; 80(9): 800 – 809. [2] Fil A et al, (2013). Parkinsonism Relat Disord; 19(3):285-94. [3] Chauduri KR et al (2015). Mov Disord; 30(12): 1623-31. [4] Rodríguez-Violante M et al (2017), Mov Disord Clin Pract; 4(4):545-551. [5] Silverdale MA et al, (2018). Parkinsonism Relat Disord; 56:27-32.
To cite this abstract in AMA style:
P. Imbriani, P. Ghosh, T. Schirinzi, N. Caputi, L. Covington, A. Sparks, Y. Salnikova, S. Natoli, A. Pisani. Relationship between pain and autonomic symptoms in Parkinson’s Disease: a double-center, cross-sectional, observational study. [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/relationship-between-pain-and-autonomic-symptoms-in-parkinsons-disease-a-double-center-cross-sectional-observational-study/. Accessed December 19, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/relationship-between-pain-and-autonomic-symptoms-in-parkinsons-disease-a-double-center-cross-sectional-observational-study/