Category: Parkinsonism, Atypical: PSP, CBD
Objective: We examined whether magnetic susceptibility estimates from deep gray matter structures in patients with Progressive Supranuclear Palsy (PSP) correlated with clinical measures of disease severity.
Background: Mineralisation and iron deposition occur in deep gray matter structures of the brain in neurodegenerative Parkinsonian disorders.[1] The topography and extent of mineralisation determined by susceptibility weighted magnetic resonance imaging techniques can differentiate PSP from healthy subjects and patients with Parkinson’s disease (PD) [2,3]. However, correlation with disease severity is not known.
Method: Patients with clinical diagnosis of probable PSP- Richardson’s syndrome underwent assessment of severity of clinical manifestations using PSP Rating Scale (PSPRS) and quantification of mineralisation of deep gray matter structures using quantitative susceptibility mapping (QSM) [4]. The magnetic susceptibility estimates were also compared with those of age-matched patients with PD and healthy volunteers. The regions of interest (ROIs) were Substantia nigra (SN), red nucleus (RN), head of caudate nucleus (CN), putamen and globus pallidus (GP).
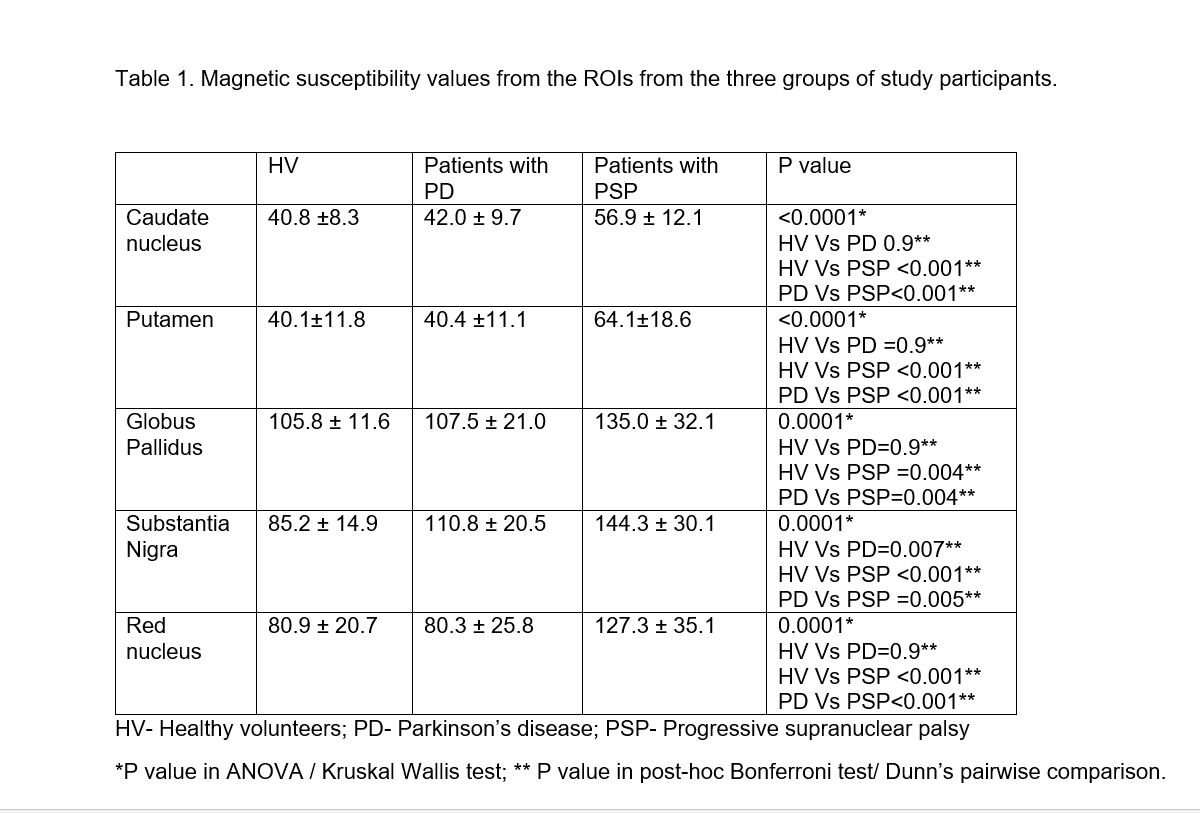
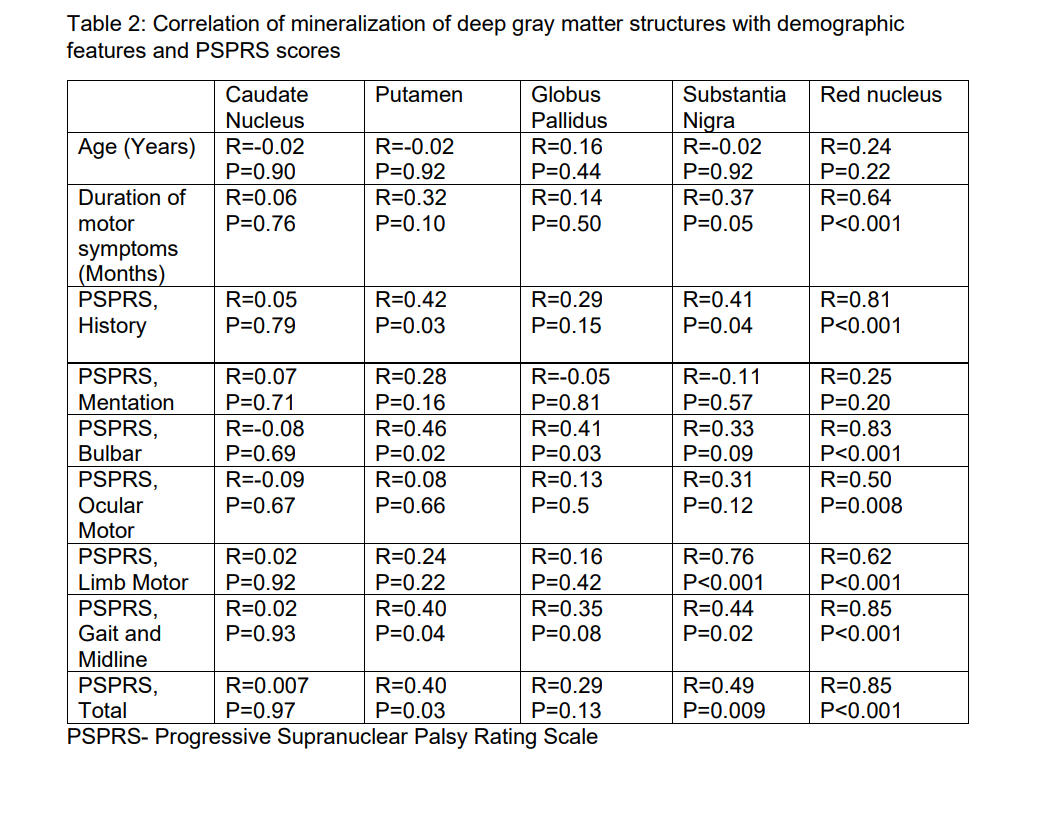
Results: The scans from 27 patients with PSP and 26 patients each in the PD and healthy volunteer groups were available for final analysis. Mineralisation in all the ROIs was significantly higher in PSP patients when compared to healthy volunteers or PD patients. [Table 1] The PSPRS scores did not correlate with mineralization in the caudate nucleus (R=0.007, P=0.97) or globus pallidus (R=0.29, P=0.13). Moderate correlation was noted between PSPRS scores and mineralization of the putamen (R=0.40, P=0.03) and substantia nigra (R=0.49, P=0.009); the scores strongly correlated with mineralisation of red nucleus (R=0.85, P<0.001). [Table 2]
Conclusion: Quantification of mineralization from basal ganglia and related structures using QSM differentiates PSP patients when compared to PD or healthy controls. Correlation with disease severity was noted for mineralization of RN, putamen and SN.
References: [1] Dexter DT, Carayon A, Javoy-Agid F, Agid Y, Wells FR, Daniel SE, et al. Alterations in the levels of iron, ferritin and other trace metals in Parkinson’s disease and other neurodegenerative diseases affecting the basal ganglia. Brain. 1991; 114(4):1953–1975.
[2] Gupta D, Saini J, Kesavadas C, Sarma PS, Kishore A. Utility of susceptibility-weighted MRI in differentiating Parkinson’s disease and atypical parkinsonism. Neuroradiology. 2010; 52(12):1087–1094.
[3] Sjöström H, Granberg T, Westman E, Svenningsson P. Quantitative susceptibility mapping differentiates between Parkinsonian disorders. Parkinsonism Relat Disord. 2017; 44:51–57.
[4] Haacke EM, Liu S, Buch S, Zheng W, Wu D, Ye Y. Quantitative susceptibility mapping: current status and future directions. Magn Reson Imaging. 2015;33(1):1–25.
To cite this abstract in AMA style:
S. Krishnan, S. George, S. Raghavan, B. Thomas, J. Thulaseedharan, D. Puthenveedu, A. Kishore. Quantitative susceptibility mapping of basal ganglia and related structures: correlation with disease severity in Progressive Supranuclear Palsy [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/quantitative-susceptibility-mapping-of-basal-ganglia-and-related-structures-correlation-with-disease-severity-in-progressive-supranuclear-palsy/. Accessed October 21, 2025.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/quantitative-susceptibility-mapping-of-basal-ganglia-and-related-structures-correlation-with-disease-severity-in-progressive-supranuclear-palsy/