Session Information
Date: Thursday, June 8, 2017
Session Title: Parkinson’s Disease: Clinical Trials, Pharmacology And Treatment
Session Time: 1:15pm-2:45pm
Location: Exhibit Hall C
Objective: To evaluate the efficacy of rotigotine transdermal patch, using a wearable sensor, to treat PD patients with nocturnal immobility.
Background: Nocturnal hypokinesia is a common night-time symptom in Parkinson’s disease (PD), negatively affecting quality of life of both patient and caregiver. However, evidence-based treatment strategies are limited.
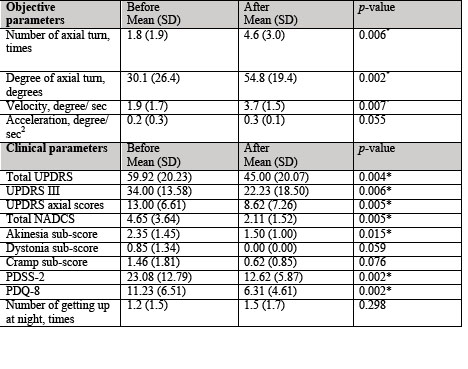
Methods: 34 PD subjects with nocturnal immobility were randomized to receive rotigotine transdermal patch (10.46+4.63 mg, 2-16 mg/24 hr, n=17) or placebo (n=17). Treatment was titrated to an optimal dose over 1-8 weeks, then maintain for 4 weeks. Primary endpoints were objective nocturnal parameters (number, velocity, acceleration, degree, and duration of turns and number of times patients got out of bed), measured using an axial inertial sensor (the NIGHT-Recorder) over two nights at the patients’ home. Correlations with validated clinical rating scales were performed.
Results: There were significant improvements in the rotigotine group in terms of number of turns in bed (p=0.006), turning velocity (p=0.007), and the degree of turning (p=0.002). Significant improvements of mean total UPDRS, mean UPDRS-III, UPDRS-axial, PDSS-2, Nocturnal Akinesia Dystonia and Cramp scale and PDQ-8 were also observed. No significant changes were observed in the placebo group. The most frequently reported adverse events were feeling discomfort over the patch area (23%), application site reactions (5.8%), and itching (5.8%).
Conclusions: Our study demonstrates rotigotine transdermal patch provides a significant improvement, compared with placebo, on both objective nocturnal outcomes and clinical rating scales. It also demonstrates the feasibility of using wearable sensors to record objective outcomes in PD-related clinical trials.
References: 1) Bhidayasiri R., Sringean J., Thanawattano C. Sensor-based evaluation and treatment of nocturnal hypokinesia in Parkinson’s disease: An evidence-based review. Parkinsonism Relat Disord 2016;22 Suppl 1:S127-33.
2) Sringean J., Taechalerpaisarn P., Thanawattano C., Bhidayasiri R. How well do Parkinson’s disease patients turn in bed? Quantitative analysis of nocturnal hypokinesia using multisite wearable inertial sensors. Parkinsonism Relat Disord 2016;23:10-6.
To cite this abstract in AMA style:
R. Bhidayasiri, J. Sringean, S. Chaiwong, C. Anan, K. Boonpang, K. Sakdisornchai, O. Jitkritsadakul, P. Jagota. Quantitative demonstration of the efficacy of rotigotine transdermal patch in the treatment of nocturnal hypokinesia: A randomized, placebo-controlled trial using an axial inertial sensor [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/quantitative-demonstration-of-the-efficacy-of-rotigotine-transdermal-patch-in-the-treatment-of-nocturnal-hypokinesia-a-randomized-placebo-controlled-trial-using-an-axial-inertial-sensor/. Accessed December 25, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/quantitative-demonstration-of-the-efficacy-of-rotigotine-transdermal-patch-in-the-treatment-of-nocturnal-hypokinesia-a-randomized-placebo-controlled-trial-using-an-axial-inertial-sensor/