Category: Parkinsonism, Atypical: PSP, CBD
Objective: PSP is traditionally considered a neurodegenerative disease of late life. Its diagnostic criteria include the item “age of onset over 40 years.” This significantly limits doctors’ ability to diagnose this disease.
Background: We present an example of our clinical case. A 37-year-old male patient came to the hospital with complaints of the inability to walk and cope with his needs.
Method: He fell ill more than one year ago, when a dysfunction of the pelvic organs, such as incontinence, suddenly appeared and he stopped walking because his “legs gave out.” He had previously been examined at several private medical centers, where he was diagnosed with multiple sclerosis. He did not receive treatment due to the development of deep bedsores. The patient was sent to the hospital for further examination.
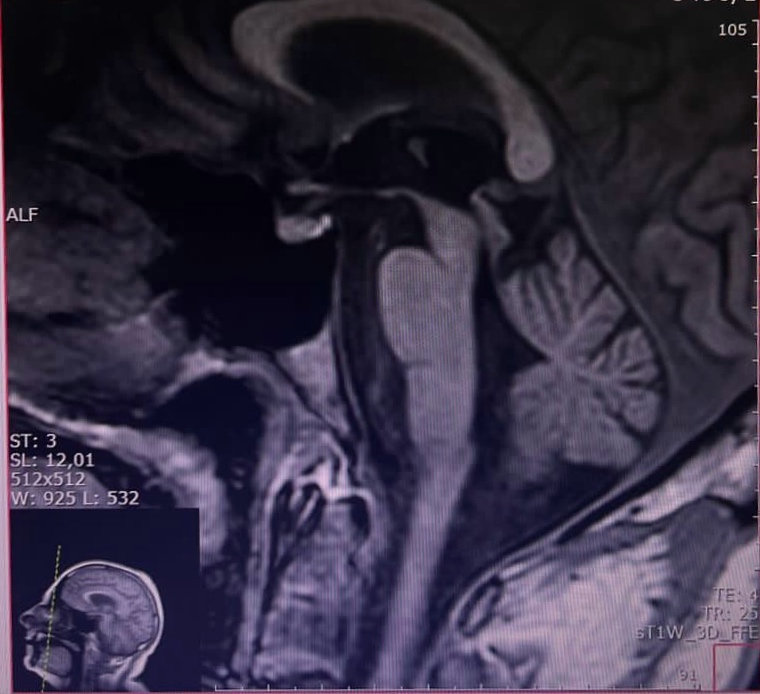
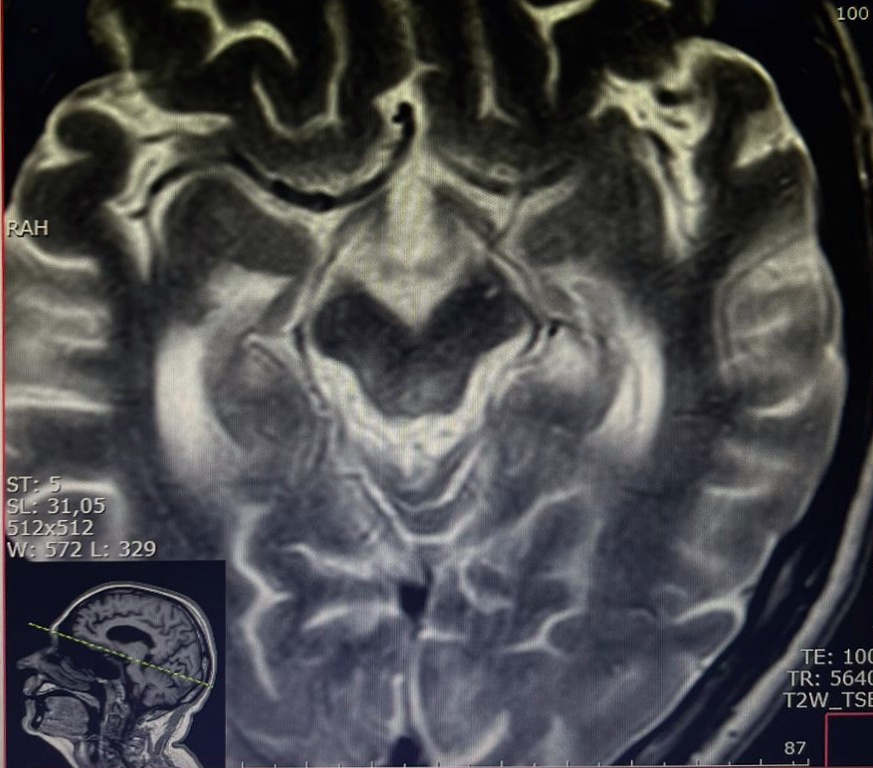
Results: During a neurological examination: the patient cannot walk, stand, sit independently, lies in a flexed position, does not move independently even within the bed, when sitting down without support falls on his back, monosyllabic speech, bradylalia, dysarthria, dysphonia, hypomimia, pharyngeal reflexes are reduced, but no dysphagia. Bradyphrenia and cognitive dysfunction up to 9 points according to MMSE. The muscle strength of the arms is 0-1 points; it is impossible to assess the strength of the muscles in the legs. Total plastic hypertonicity of the muscles of the limbs and axial muscles with the formation of retrocollis and postural reflexes. Deep reflexes are increased, there are pathological reflexes of the feet. Urinary dysfunction, such as urinary incontinence. The patient underwent an MRI of the brain: it showed a hummingbird sign and a Mickey Mouse sign.
Conclusion: This patient does not have vertical gaze palsy. His age is under 40 years old. But there is a progressive course of the disease, symmetrical rigidity and akinesia, retrocollis, dysarthria, as well as neuropsychological disorders. Therefore, despite the inconsistency of symptoms and insufficient clinical picture due to the short duration of the disease, the patient was diagnosed with PSP with corticobasal syndrome.
A hummingbird sign on patient’s MRI
A Mickey Mouse sign on patient’s MRI
To cite this abstract in AMA style:
K. Manysheva, D. Makhmudova. PSP: a Clinical Case [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/psp-a-clinical-case/. Accessed April 30, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/psp-a-clinical-case/