Category: Parkinsonism, Atypical: PSP, CBD
Objective:
This article was written to enrich the spectrum of PSP case reports, emphasizing the diagnosis aspect.
Background: Progressive supranuclear palsy (PSP) is the main cause of degenerative parkinsonism after Parkinson’s Disease (PD). The prevalence of PSP is age-dependent and estimated around 6-10% of all cases diagnosed as PD, or 6-7 cases per 100,000.
Method:
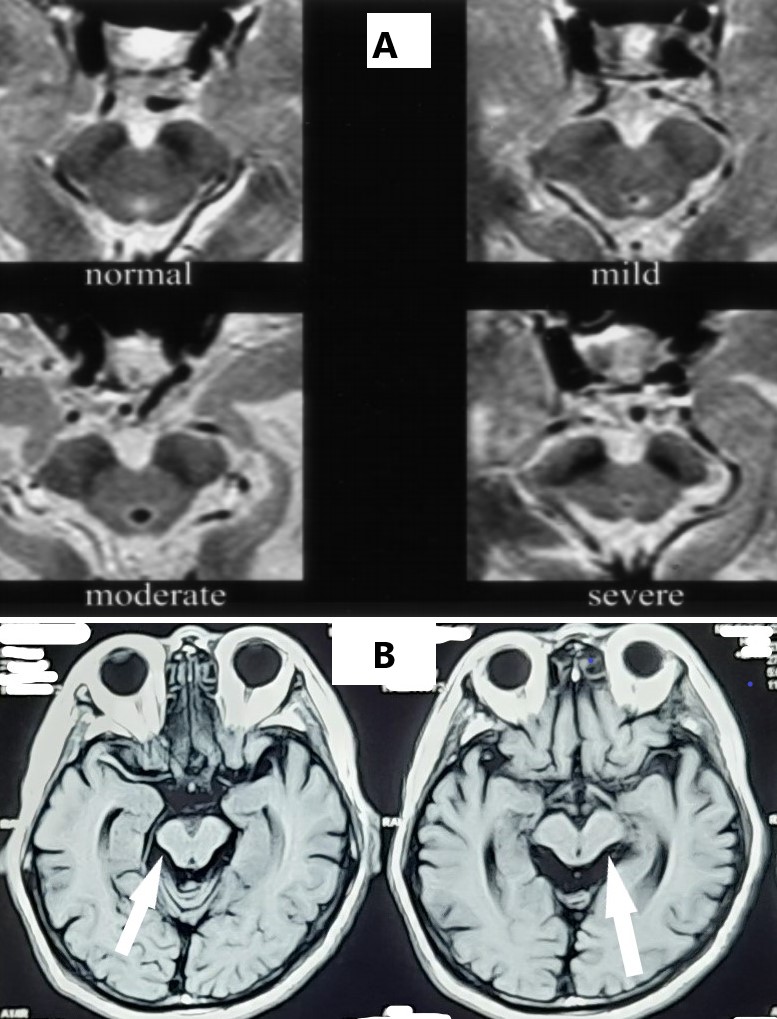
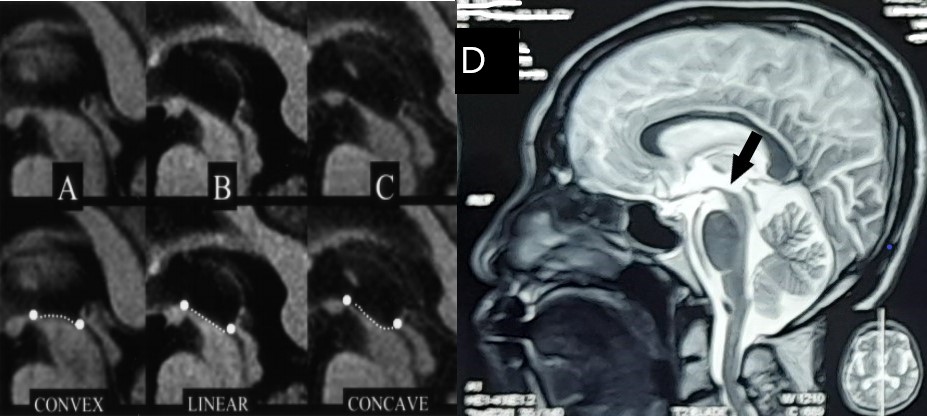
A 69-year-old male came to the neurology clinic complaining of instability of walking and tendency of sleeping for five years. He has already fallen several times, lacked of spirit, became more reserved and socially withdrawn, and got a little bit better by taking levodopa. Physical examination found dystonic posture of neck anteflexion, festinating gait, resting tremor on right extremities, bilateral vertical gaze palsy, spasticity on all extremities, and a positive retropulsion pull test. Cognitive examination showed normal function, but the patient was observed: blunt emotionally affect, losing his talking spontaneity, and decreased verbal fluency. Magnetic resonance imaging (MRI) showed midbrain atrophy, known as hummingbird sign and mickey mouse sign.
Results:
Clinical diagnosis criteria mostly used nowadays depends mostly on clinical features of vertical supranuclear gaze palsy, postural instability, and history of unexplained falling in the first year of onset. A relatively new diagnosis criteria from the Movement Disorder Society (MDS) emphasized on clinical features in four domains, which are ocular motor dysfunction, postural instability, akinesia, and cognitive dysfunction. The patient was diagnosed as probable PSP, mainly because of the vertical gaze palsy and history of unexplained falling, according to MDS criteria. MRI findings of atrophy and superior part abnormality of midbrain were good help to confirm the diagnosis.
Conclusion:
Diagnosis criteria published by MDS in 2017 helps diagnosing PSP more precisely. A precise clinical diagnosis of PSP and distinguishing it from typical PD is helpful in educating therapy and prognosis to the patient and his/her family.
References: Barsottini OGP, Felicio AC, de Aquino CCH, Pedroso JL. Progressive Supranuclear Palsy New Concepts. Arq Neuropsiquiatr. 2010;68(6):938-946.
Hoglinger GU, Respondek G, Stamelou M, Kurz C, Josephs KA, Lang AE et al. Clinical Diagnosis of Progressive Supranuclear Palsy: The Movement Disorder Society Criteria. Movement Disorders. 2017; 32(6): 853-64.
Lichter D, Koriesh A, Kapoor N, Hershey L. Progressive Supranuclear Palsy: New Diagnostic and Therapeutic Strategies. Am J Gerentol Geriatr. 2018; 1(2): 1007.
Ling H. Clinical Approach to Progressive Supranuclear Palsy. J Mov Disord. 2016; 9(1): 3-13. http://dx.doi.org/10.14802/jmd.15060.
Frank A, Peikert K, Linn J, Brandt MD, Hermann A. MDS criteria for the diagnosis of progressive supranuclear palsy overemphasize Richardson syndrome. Annals of Clinical and Translational Neurology. 2020; 7(9): 1702-1707.
Righini A, Antonini A, De Notaris R, Bianchini E, Meucci N, Sacilotto G et al. MR Imaging of the Superior Profile of the Midbrain: Differential Diagnosis between Progressive Supranuclear Palsy and Parkinson Disease. AJNR Am J Neuroradiol. 2004; 25: 927-932.
Rolland Y, Verin M, Payan CA, Duchesne S, Kraft E, Hauser TK et al. A new MRI rating scale for progressive supranuclear palsy and multiple system atrophy: validity and reliability. J Neurol Neurosurg Psychiatry. 2011; 82: 1025e1032. doi:10.1136/jnnp.2010.214890.
Quattrone A, Nicoletti G, Messina D, Fera F, Condino F, Pugliese P et al. MR Imaging Index for Differentiation of Progressive Supranuclear Palsy from Parkinson Disease and the Parkinson Variant of Multiple System Atrophy. RSNA. 2008; 246(1). https://doi.org/10.1148/radiol.2453061703.
Fatterpekar GM, Dietrich A, Pantano P, Saba L, Knopp EA, Piattella MC, Raz E. Cerebral Peduncle Angle: An Objective Criterion for Assessing Progressive Supranuclear Palsy Richardson Syndrome. AJR 2015; 205: 386-391.
Picillo M, Abate F, Ponticorvo S, Tepedino MF, Erro R, Frosini D et al. Association of MRI Measures With Disease Severity and Progression in Progressive Supranuclear Palsy. Front. Neurol. 2020; 11: 603161. doi: 10.3389/fneur.2020.603161.
To cite this abstract in AMA style:
A. Kurniadi. Progressive Supranuclear Palsy: Review On Diagnostic Aspects Based On A Case [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/progressive-supranuclear-palsy-review-on-diagnostic-aspects-based-on-a-case/. Accessed April 20, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/progressive-supranuclear-palsy-review-on-diagnostic-aspects-based-on-a-case/