Session Information
Date: Monday, June 20, 2016
Session Title: Parkinson's disease: Non-motor symptoms
Session Time: 12:30pm-2:00pm
Location: Exhibit Hall located in Hall B, Level 2
Objective: To identify the prevalence of orthostatic hypotension (OH) in early Parkinson’s disease (PD) and identify clinical features associated with greater postural drop in BP in PD.
Background: Orthostatic hypotension is common in advanced PD but its prevalence is unclear as is the extent to which it symptomatically affects patients with early disease and the time course over which it develops.
Methods: Between June 2009 and December 2011, 158 subjects with newly diagnosed PD and 99 age-matched controls were recruited to the Newcastle arm of a longitudinal observational study examining the characteristics of early PD. Participants underwent comprehensive clinical assessment including assessment of lying and standing blood pressure (BP) and symptoms of postural dizziness. Assessments were repeated at 18 and 36 months follow-up. Orthostatic hypotension was defined according to consensus criteria as a drop of 20mmHg or more in systolic BP and/or a drop of 10mmHg in diastolic BP. Prevalence of OH at each time point was examined and mixed effects modelling was used to examine the effect of disease duration, disease severity, medication and cardiovascular risk factors on systolic vasodepression among participants with PD.
Results: At baseline and at 18 months the prevalence of OH did not significantly differ between subjects and controls. At 36 months OH was significantly more common among subjects with PD than age matched controls. 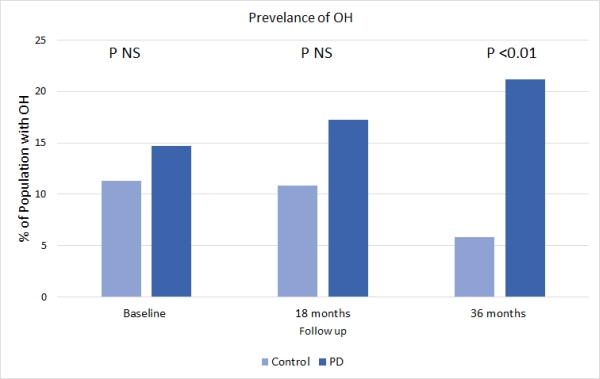 By 36 months, 43% of PD cases with OH were symptomatic and 3 subjects were prescribed fludrocortisone. Mixed effects modelling showed that, in addition to disease duration, greater systolic vasodepression was independently associated with a history of postural dizziness (p<0.05), and low BMI (p<0.05). Vasodepression was not associated with age, severity of motor symptoms, levodopa equivalent dose (LED), or use of antihypertensive medication.
By 36 months, 43% of PD cases with OH were symptomatic and 3 subjects were prescribed fludrocortisone. Mixed effects modelling showed that, in addition to disease duration, greater systolic vasodepression was independently associated with a history of postural dizziness (p<0.05), and low BMI (p<0.05). Vasodepression was not associated with age, severity of motor symptoms, levodopa equivalent dose (LED), or use of antihypertensive medication.
Conclusions: Orthostatic hypotension affects over 20% of patients with PD within the first 3 years from diagnosis. Greater systolic vasodepression was associated with a clinical history of postural dizziness suggesting it is clinically significant to the patient. The failure to identify an association between the degree of vasodepression and severity of motor features suggests that OH may progress independently of motor disease. In this study LED was not significantly associated with OH indicating that it may not be a significant contributor to OH in patients with early PD.
To cite this abstract in AMA style:
C. McDonald, R.A. Lawson, G.W. Duncan, T.K. Khoo, D.J. Brooks, R.A. Barker, A.J. Yarnall, D.J. Burn. Prevalence and risk factors for orthostatic hypotension in early PD [abstract]. Mov Disord. 2016; 31 (suppl 2). https://www.mdsabstracts.org/abstract/prevalence-and-risk-factors-for-orthostatic-hypotension-in-early-pd/. Accessed December 28, 2025.« Back to 2016 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/prevalence-and-risk-factors-for-orthostatic-hypotension-in-early-pd/
