Category: Parkinson's Disease: Non-Motor Symptoms
Objective: Identify predictors of relapse in impulse control disorders (ICD) in patients with Parkinson’s disease.
Background: Behaviors that are performed repeatedly, excessively or minimally and compulsively can interfere with the functionality of the patient with Parkinson’s Disease, these behaviors have been defined as Impulse Control Disorders. However, there is great variability in prevalence reports; This has been related to social, cultural and economic factors. Usually the risk of this has been related to the use of dopaminergic drugs, early age of diagnosis and a history of depressive symptoms. Therefore, its evaluation is complex and requires a treatment focused on pharmacological and non-pharmacological measures.
Method: Retrospective study, carried out at the National Institute of Neurology and Neurosurgery of Mexico City from 2018 to 2020. The patients exhibited a follow-up of 3 neurological consultations.The Questionnaire for Impulsive-Compulsive Disorders (QUIPS), a validated tool for diagnosing or establishing risk of impulse control disorder, was used. A comparative analysis was performed using a Wilcoxon test for related variables, a p<0.05 was considered a significant result.
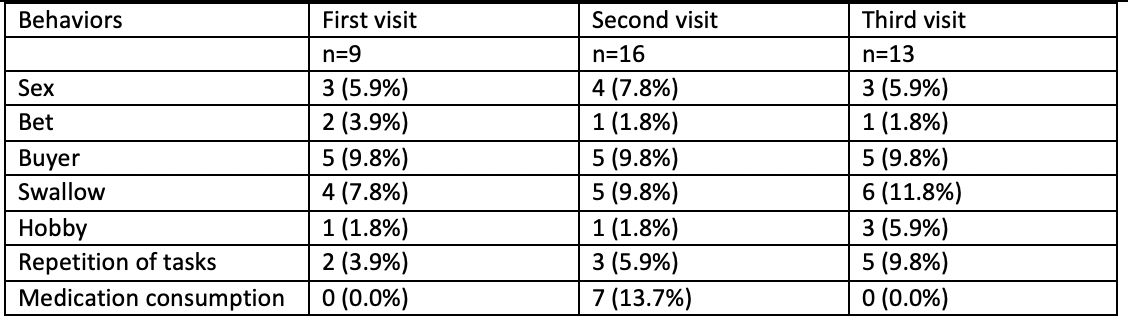
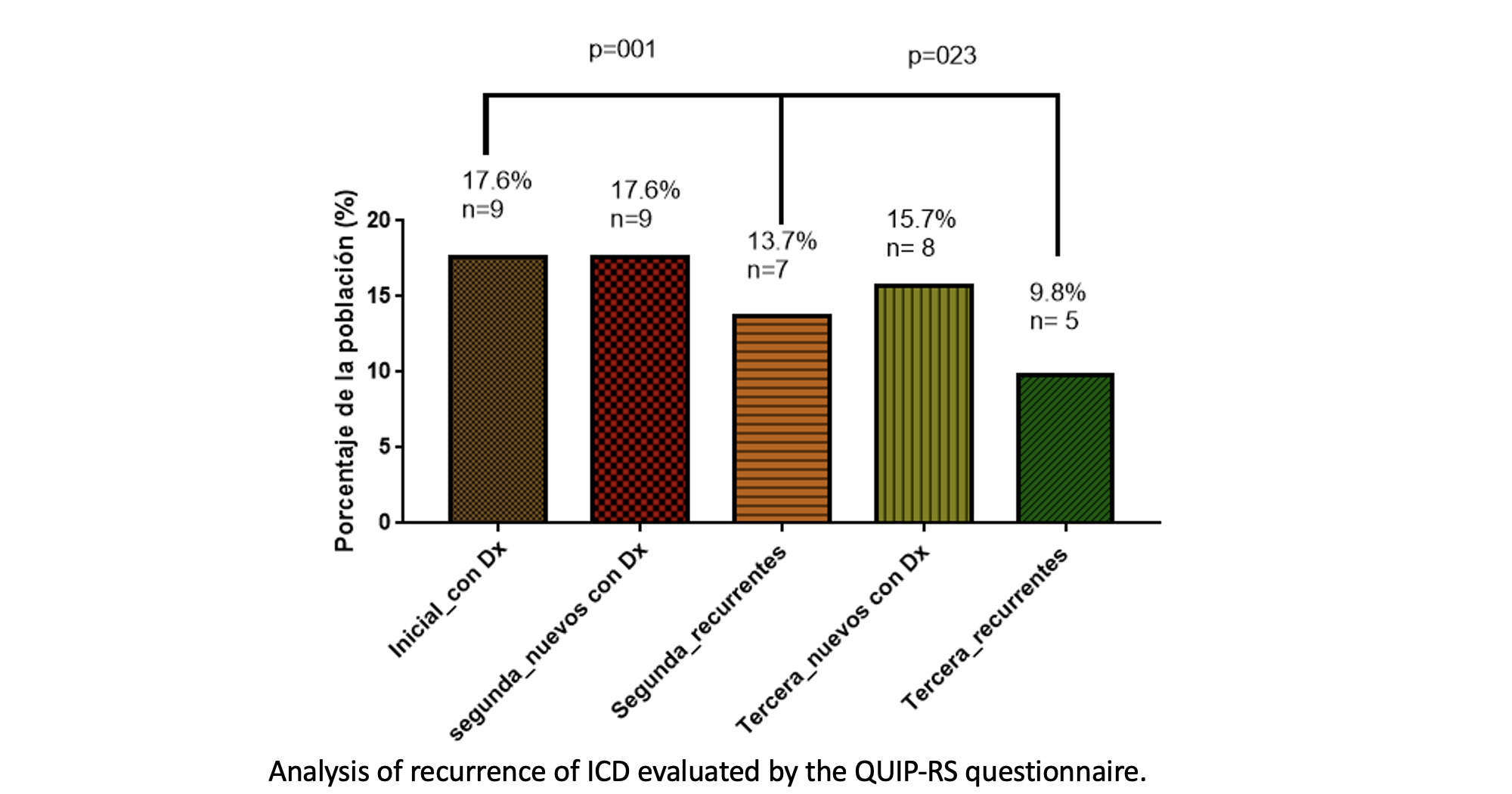
Results: The percentage of patients with Impulse Control Disorder according to the evaluation was 17.6% (9/51) for the first consultation 31.3% (16/51) for the second and 25.4% (13/51) for the third. Specifically, during the second consultation, 13.7% (7/51%) of the patients presented compulsion for medications. Likewise 9.8% (5/51) patients persisted with TCI during the course of the study despite therapeutic modifications (p<0.05) eating and shopping behaviors prevailed. Other risk factors such as age clinical stage use of dopaminergic agonists or deep stimulation were not related to impulse control disorder (p>0.05).
Conclusion: The percentage of ICD in the population was significant in the three consultations (17.6%, 31.3% and 25.4%) a high percentage of persistence of ICD is maintained in this population 9.8%. This could be related to the different indications of other authors where they have described structural and/or genetic alterations that due to the nature of the present could not be described.
References: 1. Martínez-Jurado E, Cervantes-Arriaga A, Rodríguez-Violante M. Quality of life in patients with Parkinson’s disease. Rev Mex Neurocienc. 2010;11(6):480–6.
2. Weintraub D, David AS, Evans AH, Grant JE, Stacy M. Clinical spectrum of impulse control disorders in Parkinson’s disease: SPECTRUM OF IMPULSE CONTROL DISORDERS
IN PD. Mov Disord. febrero de 2015;30(2):121–7.
3. Elizabeth M-J, Amin C-A, Mayela R-V. Calidad de vida en pacientes con enfermedad de Parkinson.
:7.
4. Campo Arias A, Castillo Támara EE, Herazo E. Revisión de casos de zoofilia en pacientes con enfermedad de Parkinson. Rev Neurol. 2018;67(04):129.
5. Seeman P, Van Tol HH. Dopamine receptor pharmacology. Curr Opin Neurol Neurosurg. agosto de 1993;6(4):602–8.
6. Richtand NM, Woods SC, Berger SP, Strakowski SM. D3 dopamine receptor, behavioral sensitization, and psychosis. Neurosci Biobehav Rev. julio de 2001;25(5):427–43.
7. Parkinson J. An essay on the shaking palsy. 1817. J Neuropsychiatry Clin Neurosci. 2002;14(2):223–36; discussion 222.
8. Armstrong MJ, Okun MS. Diagnosis and Treatment of Parkinson Disease: A Review. JAMA. el 11 de febrero de 2020;323(6):548.
9. rizo curiel G, Villaseñor-Cabrera T, Jarne-Esparcia A, Zuñiga-Ramírez C, Soto-Escageda A. Factores de riesgo para desarrollar Trastorno del control de los impulsos en
Enfermedad de Parkinson. el 1 de octubre de 2018;10:9–14.
10. Weintraub D, Claassen DO. Impulse Control and Related Disorders in Parkinson’s Disease. En: International Review of Neurobiology [Internet]. Elsevier; 2017 [citado el 28 de junio de 2021]. p. 679–717. Disponible en: https://linkinghub.elsevier.com/retrieve/pii/S0074774217300363
11. Rodríguez-Violante M, González-Latapi P, Cervantes-Arriaga A, Camacho-Ordoñez A, Weintraub D. Impulse control and related disorders in Mexican Parkinson’s disease
patients. Parkinsonism Relat Disord. agosto de 2014;20(8):907–10.
12. Abstracts. Mov Disord Clin Pract [Internet]. febrero de 2020 [citado el 29 de junio de 2021];7(S1). Disponible en: https://onlinelibrary.wiley.com/doi/abs/10.1002/mdc3.12905
13. Drew DS, Muhammed K, Baig F, Kelly M, Saleh Y, Sarangmat N, et al. Dopamine and reward hypersensitivity in Parkinson’s disease with impulse control disorder. Brain. el 1 de
agosto de 2020;143(8):2502–18.
14. Goodwin FK. Psychiatric Side Effects of Levodopa in Man. JAMA. el 27 de diciembre de 1971;218(13):1915–20.
15. Djamshidian A, O’Sullivan SS, Wittmann BC, Lees AJ, Averbeck BB. Novelty seeking behaviour in Parkinson’s disease. Neuropsychologia. julio de 2011;49(9):2483–8.
16. Phu AL, Xu Z, Brakoulias V, Mahant N, Fung VSC, Moore GD, et al. Effect of impulse control disorders on disability and quality of life in Parkinson’s disease patients. J Clin
Neurosci. el 1 de enero de 2014;21(1):63–6.
17. Antonini A, Cilia R. Behavioural adverse effects of dopaminergic treatments in Parkinson’s disease: incidence, neurobiological basis, management and prevention. Drug Saf.
2009;32(6):475–88.
18. Roussakis A, Lao–Kaim NP, Piccini P. Brain Imaging and Impulse Control Disorders in Parkinson’s Disease. Curr Neurol Neurosci Rep. septiembre de 2019;19(9):67.
19. Gatto EM, Aldinio V. Impulse Control Disorders in Parkinson’s Disease. A Brief and Comprehensive Review. Front Neurol. el 17 de abril de 2019;10:351.
20. Tippmann-Peikert M, Park JG, Boeve BF, Shepard JW, Silber MH. Pathologic gambling in patients with restless legs syndrome treated with dopaminergic agonists. Neurology. el
23 de enero de 2007;68(4):301–3.
21. Weintraub D, Claassen DO. Impulse Control and Related Disorders in Parkinson’s Disease. International Review of Neurobiology. 2017;133:679–717.
22. Arango Uribe GJ, Bernal Pacheco O. Trastorno de control de impulsos (TCI) en enfermedad de Parkinson. Acta Neurológica Colomb. el 20 de agosto de 2019;35(3 supl. 1):2832.
To cite this abstract in AMA style:
L. Gaibor, D. Vazquez, H. Estrada. Predictors of relapse in impulse control disorders in patients with Parkinson’s disease. [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/predictors-of-relapse-in-impulse-control-disorders-in-patients-with-parkinsons-disease/. Accessed January 2, 2026.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/predictors-of-relapse-in-impulse-control-disorders-in-patients-with-parkinsons-disease/