Session Information
Date: Monday, September 23, 2019
Session Title: Psychiatric Manifestations
Session Time: 1:45pm-3:15pm
Location: Les Muses Terrace, Level 3
Objective: To identify predictive factors for depression in a multicentric Parkinson’s disease (PD) mexican cohort.
Background: Depression is a common symptom of PD with a reported prevalence varying between 2.7% and 90%(1, 2). Around 40% have significant depressive symptoms. Depression has a negative impact on patient’s quality of life(3).
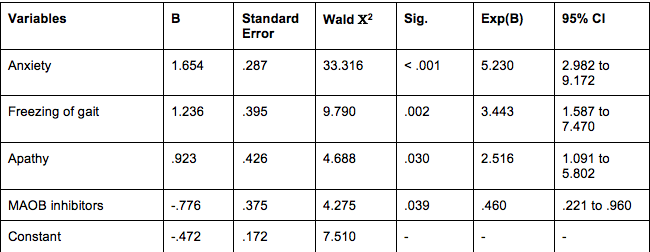
Method: Cross-sectional analytical study of PD patients from a multicentric mexican PD cohort (n=306) evaluated in 2017-2018. Demographic and clinical variables were documented as predictive variables and depression as the outcome. Variables with significant association were used to construct multivariate regression model to determine predictive factors {table 1}.
Results: 57.8% (177/306) reported depressive symptoms. Right-sided symptom onset (OR = 1.72, P = .020), PIGD subtype (OR 2.19, P = .001), HY III-IV (OR = 4.21, P = .006), MDS-UPDRS part III (MD = -5.58, P = .002), presence of cognitive impairment (OR = 1.89, P = .007), psychosis (OR = 1.99, P = .030), anxiety (OR = 5.56, P = <.001), apathy (OR 4.41, P= <.001), sleep problems (OR = 1.72, P = .020), pain (OR 1.88, P = .007), drooling (OR = 2.01, P = .033), gait problems (OR = 2.30, P = .002), and freezing of gait (OR = 3.23, P = .001) were significantly associated with depression. Multivariate analysis proved the presence of apathy (beta = 2.52, P = 0.030), freezing of gait (beta = 3.44, P = .002), and anxiety (beta = 5.23, P = <.001) to be significant predictors for depression. MAOB inhibitors were found to be a protective factor for depression (beta = 0.46, P = 0.039). [table1] When comparing MAOB inhibitors, selegiline was associated with lower presence of depression compared to rasagiline (OR = 0.19, P = 0.022). The model showed an accuracy of 71.9%, sensitivity 79.4%, specificity 64.2%, PPV 69.5%, and NPV 75.2%.
Conclusion: Prevalence and associated factors with depression are congruent with previously reported data. Treating apathy, freezing of gait, and anxiety might improve depression. Better design studies are needed to confirm our results.
References: 1. Timmer MHM, van Beek M, Bloem BR, Esselink RAJ. What a neurologist should know about depression in Parkinson’s disease. Pract Neurol. 2017;17(5):359-68. 2. Isais-Millan S, Pina-Fuentes D, Guzman-Astorga C, Cervantes-Arriaga A, Rodriguez-Violante M. [Prevalence of neuropsychiatric disorders in drug-naive subjects with Parkinson’s disease (PD)]. Gac Med Mex. 2016;152(3):357-63. 3. Rodriguez-Violante M, Cervantes-Arriaga A, Corona T, Martinez-Ramirez D, Morales-Briceno H, Martinez-Martin P. Clinical determinants of health-related quality of life in Mexican patients with Parkinson’s disease. Arch Med Res. 2013;44(2):110-4.
To cite this abstract in AMA style:
A. Banegas-Lagos, A. Cervantes-Arriaga, D. Garza-Brambila, E. Garcia-Berlanga, K. Salinas-Barboza, S. Isais-Millan, A. Anaya-Escamilla, E. Velazquez-Avila, G. Parra, A. Gonzalez-Cantú, M. Rodriguez-Violante, D. Martinez-Ramirez. Predictive Factors for Depression in a Multicentric Parkinson’s Disease Mexican Cohort [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/predictive-factors-for-depression-in-a-multicentric-parkinsons-disease-mexican-cohort/. Accessed January 2, 2026.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/predictive-factors-for-depression-in-a-multicentric-parkinsons-disease-mexican-cohort/