Objective: Investigate the use of potentially inappropriate medications (PIM) among patients newly diagnosed with dementia with Lewy bodies (DLB).
Background: PIM, including anticholinergics, are associated with increased risk of delirium, hospitalization, falls, frailty, and mortality among patients with dementia. [1]
Method: We analyzed electronic health records and claims data between October 2015 and November 2022 in an integrated US healthcare system. Member-patients diagnosed with DLB or Alzheimer’s disease (AD) were included. Controls without a cognitive diagnosis were matched (3:1) on age/sex to the DLB group. The number of unique PIM from the 2019 Beers Criteria [2] and Anticholinergic Cognitive Burden Scale (ACB) scores were calculated for 12-months pre-and post-index (e.g., the first date with a dementia diagnosis). Logistic regression adjusting for age, sex, race, and comorbidities was used to estimate the odds of ≥1 PIM and/or ACB score ≥2 for the entire observation period.
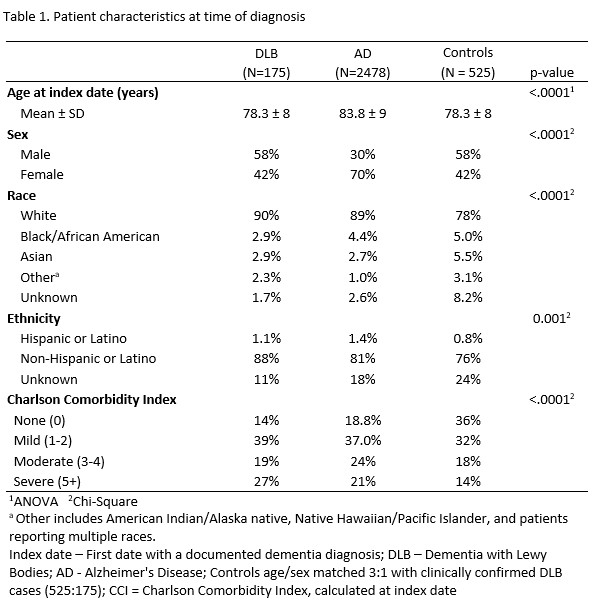
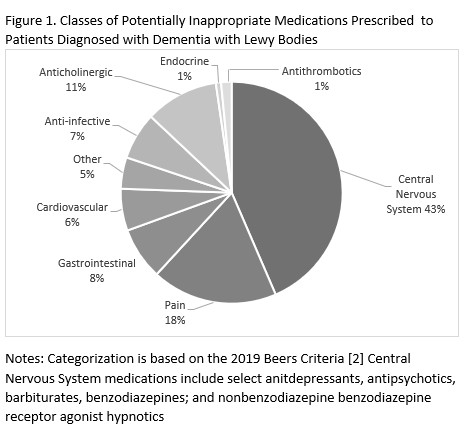
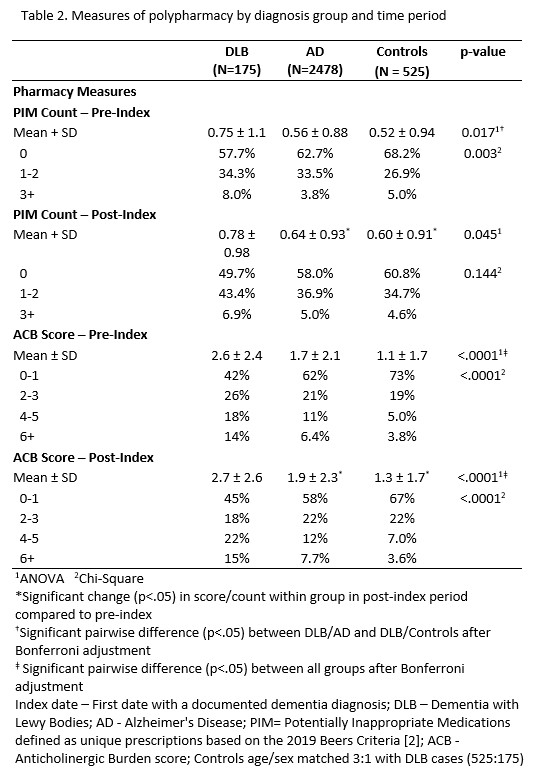
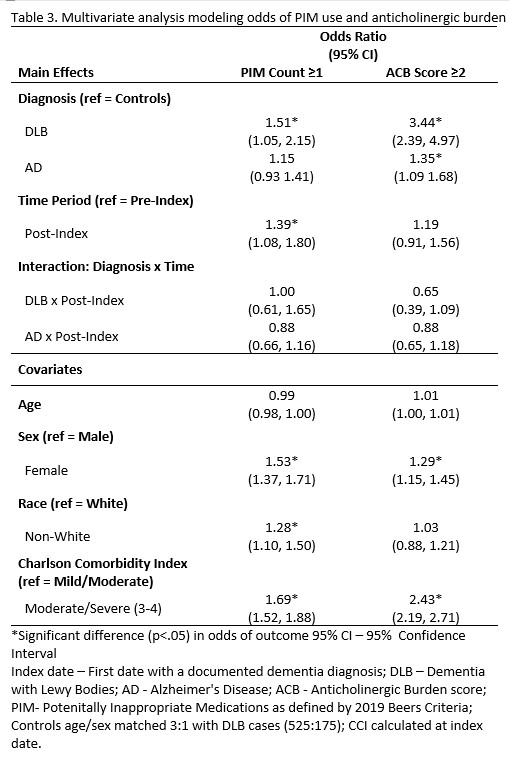
Results: DLB (n=175) and matched control (n=525) groups were significantly younger (78.3±8 vs. 83.8±9) with a higher proportion of men (58% vs. 30%) than the AD group (n=2478; p<.001). [table1] During both time periods, the DLB group had the highest number of PIM (p<.001). Central nervous system drugs (e.g., benzodiazepines, antipsychotics, and select antidepressants categorized by the Beers criteria), were the most frequent PIM prescriptions for patients with DLB. [figure1] Pre-index, 14% of patients with DLB had an ACB score of 6+ compared to 6.4% of patients with AD and 3.8% of controls (p<.001). Post-index, patients with DLB were also more likely to have an ACB score of 6+ (15%) compared to AD (7.7%) and control (3.6%) groups (p<.001). DLB and AD groups were significantly more likely to have ACB scores ≥2 compared to controls. [table2] The ACB score did not change from pre-to post-index for patients with DLB. After adjustment for demographics, the DLB group had 51% greater odds of ≥1 PIM over the total observation period than controls. There were significantly higher odds of ≥1 PIM in the post-index period for all 3 groups (OR:1.39 95% 1.08, 1.80). [table3]
Conclusion: Patients with DLB had high rates of PIM usage and anticholinergic burden prior to a dementia diagnosis. Results support deprescribing interventions at the time of diagnosis. Generalizability may be limited given the use of data from one healthcare system.
References: [1] Vickers LE, Martinez AI, Wallem AM, Johnson C, Moga DC. Potentially Inappropriate Medication Use in Older Adults with Alzheimer’s Disease and Related Dementias Living in the Community: A Cross-Sectional Analysis. Drugs Real World Outcomes. 2021;8(4):519-526. doi:10.1007/s40801-021-00265-4
[2] American Geriatrics Society 2019 updated AGS Beers Criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2012; 60(4): 616- 631.
To cite this abstract in AMA style:
K. Wyman-Chick, E. Chrenka, M. Barrett, M. Miller, L. Sargent, J. Kuntz, H. Nguyen, A. Werner, Z. Libert, R. Rossom. Potentially inappropriate medication useage among patients newly diagnosed with dementia with Lewy bodies [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/potentially-inappropriate-medication-useage-among-patients-newly-diagnosed-with-dementia-with-lewy-bodies/. Accessed February 1, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/potentially-inappropriate-medication-useage-among-patients-newly-diagnosed-with-dementia-with-lewy-bodies/