Category: Choreas (Non-Huntington's Disease)
Objective: To report a clinical manifestation of severe choreoballistic movement in a patient with anti-glial fibrillary acidic protein (GFAP) antibody positive autoimmune encephalitis
Background: GFAP is a recently identified autoantigen as a biomarker of the novel autoimmune central nervous system disorder. Movement disorders in autoimmune GFAP encephalitis have been rarely reported presenting as ataxia or tremor combined with epilepsy, cognitive or psychiatric manifestations, or myelopathy.
Method: Case report
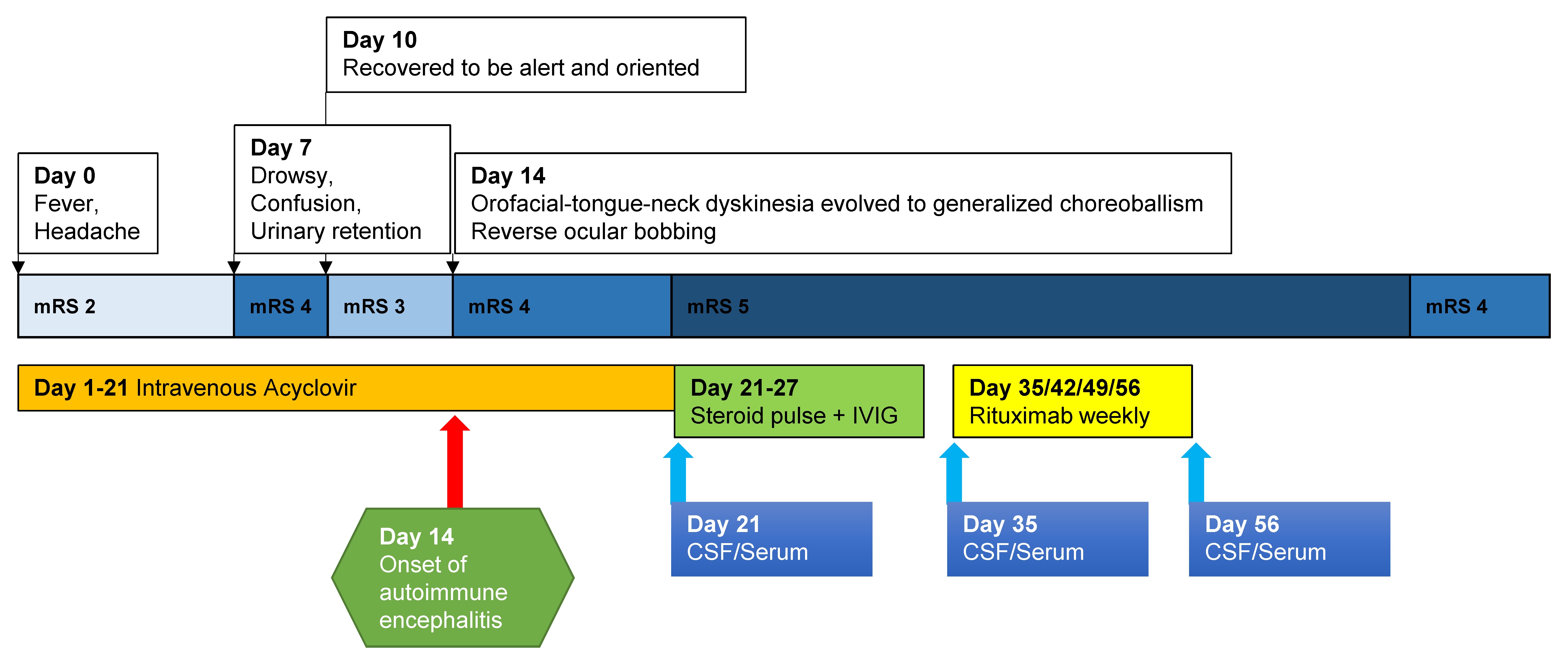
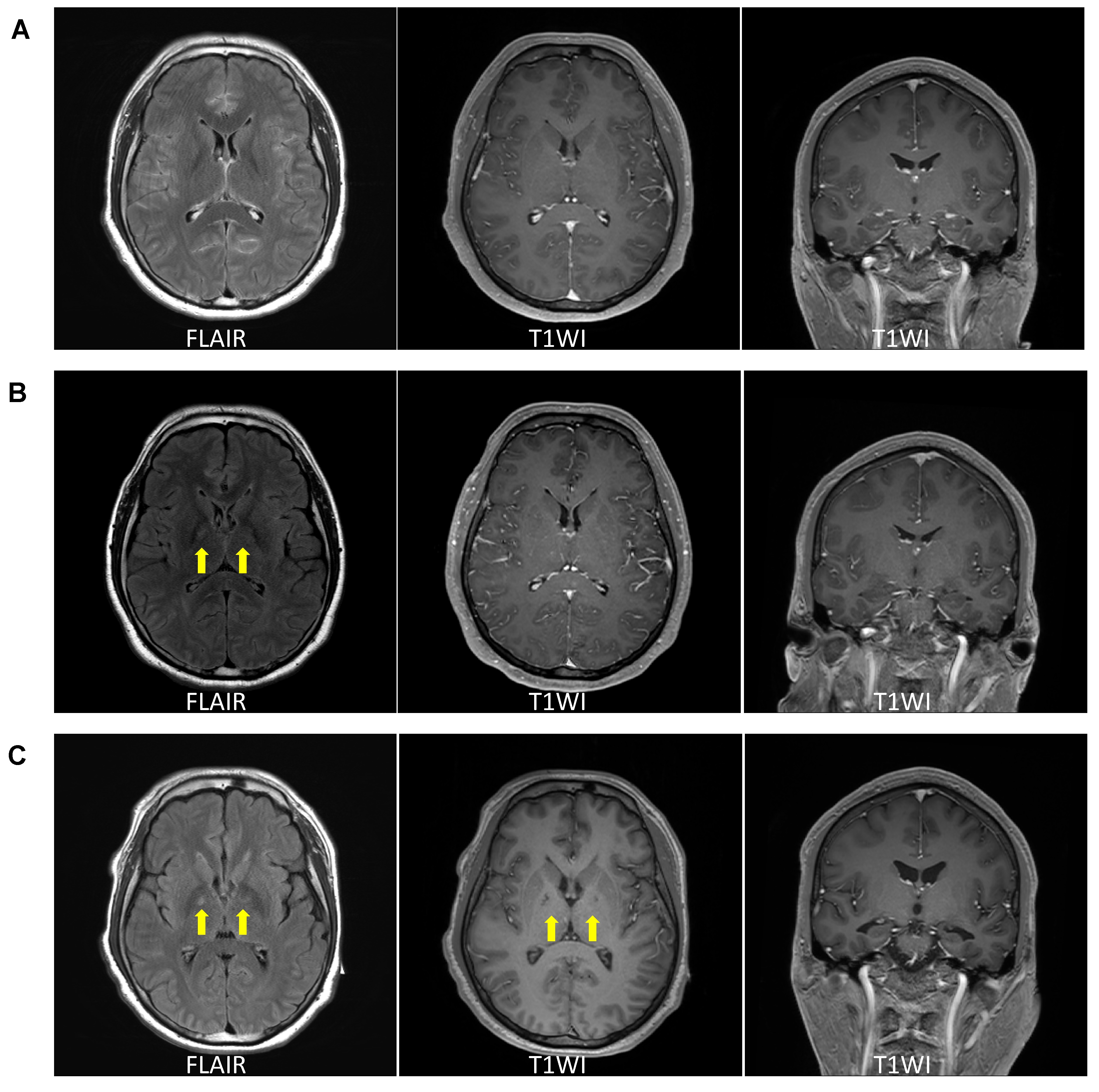
Results: A 32-year-old man complained of headache and fever from 2 days ago (Day 0, Figure 1). Cerebrospinal fluid (CSF) profiles indicated viral meningitis in which lymphocyte-dominant leukocytosis, elevated protein concentration, and normal range of glucose. Brain MRI revealed diffuse meningeal enhancement along the both cerebral sulci (Figure 2A). Under the empirical acyclovir treatment, he became rapidly aggravated showing drowsiness, confusion, and urinary retention (Day 7). We treated him with intravenous dexamethasone, empirical antibiotics, and anti-tuberculosis medications, and he gradually improved to be alert and oriented without motor or sensory deficits. At Day 14 from illness, he suddenly developed orofacial, tongue, and neck dyskinesia with reverse ocular bobbing which evolved to continuous generalized choreoballism over the following week. Severe dyskinesia was only managed with continuous infusion of sedatives and neuromuscular blockers. Brain MRI showed subtle hypersignal intensity at bilateral globus pallidus interna (GPi) on the fluid attenuated inversion recovery (FLAIR) (Figure 2B). Although the test of herpes virus was negative in all CSF examinations and other etiologies were excluded, the clinical picture certainly suggested an acute inflammatory trigger of a secondary process reminding of post-herpetic autoimmune encephalitis. We tried to immunomodulatory therapies for a month with regular lumbar punctures. Anti-neuronal antibody tests resulted in positive against GFAP with the strongest reactivity in the CSF before treatment. Dyskinesia was gradually improved and tolerable with oral medications. Follow-up brain MRI showed prominent hypersignal intensity at bilateral GPi on FLAIR with hyposignal intensity on T1-weighted images (Figure 2C).
Conclusion: This case showed a post-infectious GFAP meningoencephalitis with uncommon clinical presentation and imaging findings.
To cite this abstract in AMA style:
T. Ahn, J. Joo. Post-infectious Anti-GFAP-associated meningoencephalitis: A case report [abstract]. Mov Disord. 2021; 36 (suppl 1). https://www.mdsabstracts.org/abstract/post-infectious-anti-gfap-associated-meningoencephalitis-a-case-report/. Accessed April 17, 2025.« Back to MDS Virtual Congress 2021
MDS Abstracts - https://www.mdsabstracts.org/abstract/post-infectious-anti-gfap-associated-meningoencephalitis-a-case-report/