Category: Parkinsonism, Others
Objective: We performed a critical appraisal of the COVID-19-related parkinsonism cases reported in the literature so far, providing a phenomenological and diagnostic framework based on current diagnostic criteria.
Background: Covid-19 pandemic has shown that SARS-CoV-2 infection is associated with different neurologic manifestations, including cases of parkinsonism. A close temporal relationship between infection and new onset of parkinsonism was reported, but evidence of a causal relationship is still lacking [1]. Quality of reports is certaintly a key factor for understanding the connection between Covid-19 and parkinsonism.
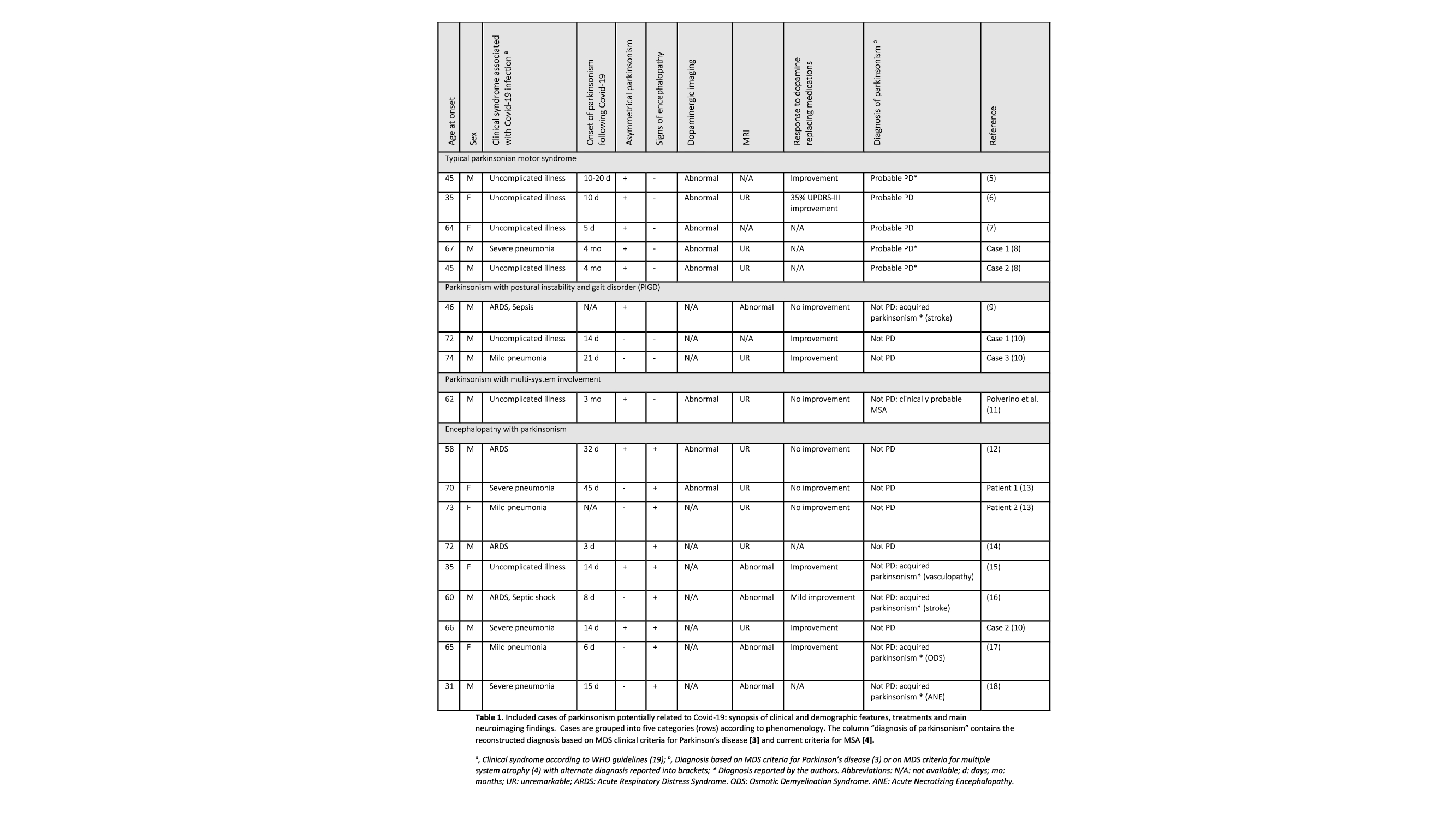
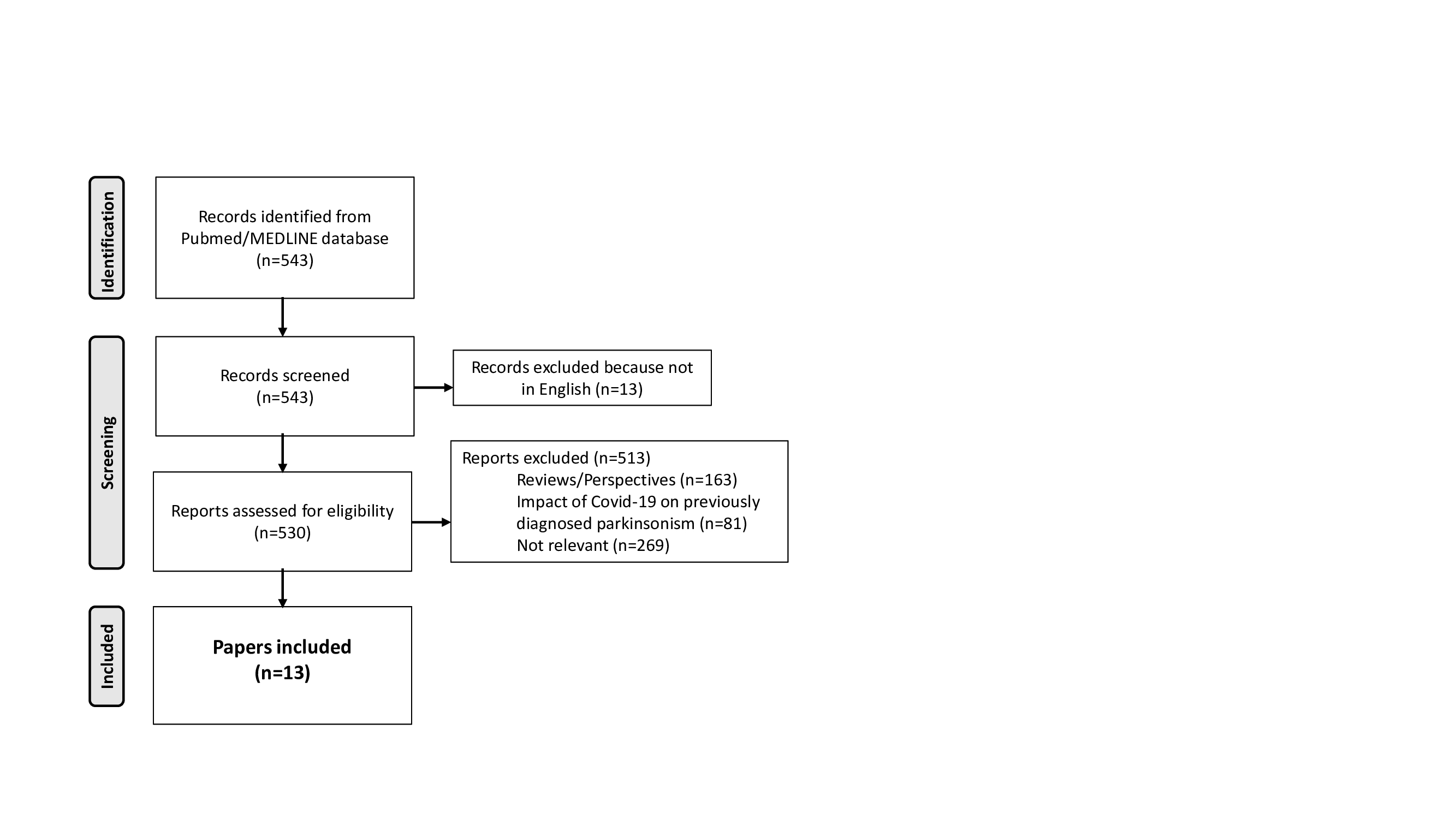
Method: A comprehensive PubMed search was conducted for cases of parkinsonism occurring in temporal connection with Covid-19 published until December 2022 [figure1]. The methodological quality of reports was assessed by two independent reviewers, applying a tool assessing different domains [2]. PD and MSA were diagnosed based on consensus MDS criteria [3,4]. Reports were grouped into consistent phenomenological sets.
Results: The search strategy identified 17 cases of parkinsonism following a confirmed SARS-CoV-2 infection encompassing a clinically heterogeneous collection of reports [5-18] [table1]. The quality of reports was assessed as low in 7 cases (39%), moderate in 6 (33%), high in 5 (28%). Cases were grouped into four consistent categories according to phenomenology: typical parkinsonian motor syndrome (5), parkinsonism with postural instability and gait disorder (3), parkinsonism with multi-system involvement (1) encephalopathy with parkinsonism (9). After criteria application 5 patients matched criteria for clinically probable PD, 1 for clinically probable MSA. Other cases were assessed as acquired parkinsonism or unclassified.
Conclusion: Evidence of a causal relationship between SARS-CoV-2 infection and parkinsonism is lacking in most of the cases, raising the possibility of a coincidental occurrence. SARS-CoV-2 infection may otherwise have acted as an environmental trigger to facilitate onset or progression of parkinsonism. Despite its limitations, this exercise emphasizes the limit of several publications where the insufficient quality of report does not allow to extend this evidence in clinical practice. Prospective cohort studies are needed to observe the real impact of Covid-19 on a potential rise in parkinsonism.
References: 1. Li WS, Chan LL, Chao YX, Tan EK. Parkinson’s disease following COVID-19: causal link or chance occurrence? J Transl Med. 2020;18(1):493.
2. Murad MH, Sultan S, Haffar S, Bazerbachi F. Methodological quality and synthesis of case series and case reports. BMJ Evid Based Med. 2018;23(2):60-3.
3. Postuma RB, Berg D, Stern M, Poewe W, Olanow CW, Oertel W, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord. 2015;30(12):1591-601.
4. Wenning GK, Stankovic I, Vignatelli L, Fanciulli A, Calandra-Buonaura G, Seppi K, et al. The Movement Disorder Society Criteria for the Diagnosis of Multiple System Atrophy. Mov Disord. 2022;37(6):1131-48.
5. Cohen ME, Eichel R, Steiner-Birmanns B, Janah A, Ioshpa M, Bar-Shalom R, et al. A case of probable Parkinson’s disease after SARS-CoV-2 infection. Lancet Neurol. 2020;19(10):804-5.
6. Faber I, Brandao PRP, Menegatti F, de Carvalho Bispo DD, Maluf FB, Cardoso F. Coronavirus Disease 2019 and Parkinsonism: A Non-post-encephalitic Case. Mov Disord. 2020;35(10):1721-2.
7. Makhoul K, Jankovic J. Parkinson’s disease after COVID-19. J Neurol Sci. 2021;422:117331.
8. Cavallieri F, Fioravanti V, Toschi G, Grisanti S, Napoli M, Moratti C, et al. COVID-19 and Parkinson’s disease: a casual association or a possible second hit in neurodegeneration? J Neurol. 2022;269(1):59-61.
9. Fearon C, Mikulis DJ, Lang AE. Parkinsonism as a Sequela of SARS-CoV-2 Infection: Pure Hypoxic Injury or Additional COVID-19-Related Response? Mov Disord. 2021;36(7):1483-4.
10. Rao AR, Hidayathullah SM, Hegde K, Adhikari P. Parkinsonism: An emerging post COVID sequelae. IDCases. 2022;27:e01388.
11. Polverino P, De Santis T, Perdixi E, Chio A, Albanese A. A case of atypical parkinsonism following SARS-CoV-2 infection: casuality or causality? Unpublished data.
12. Mendez-Guerrero A, Laespada-Garcia MI, Gomez-Grande A, Ruiz-Ortiz M, Blanco-Palmero VA, Azcarate-Diaz FJ, et al. Acute hypokinetic-rigid syndrome following SARS-CoV-2 infection. Neurology. 2020;95(15):e2109-e18.
13. Morassi M, Palmerini F, Nici S, Magni E, Savelli G, Guerra UP, et al. SARS-CoV-2-related encephalitis with prominent parkinsonism: clinical and FDG-PET correlates in two patients. J Neurol. 2021;268(11):3980-7.
14. Akilli NB, Yosunkaya A. Part of the Covid19 puzzle: Acute parkinsonism. Am J Emerg Med. 2021;47:333 e1- e3.
15. Ayele BA, Demissie H, Awraris M, Amogne W, Shalash A, Ali K, et al. SARS-COV-2 induced Parkinsonism: The first case from the sub-Saharan Africa. Clin Park Relat Disord. 2021;5:100116.
16. Roy D, Song J, Awad N, Zamudio P. Treatment of unexplained coma and hypokinetic-rigid syndrome in a patient with COVID-19. BMJ Case Rep. 2021;14(3).
17. Ghosh R, Ray A, Roy D, Das S, Dubey S, Benito-Leon J. Parkinsonism with akinetic mutism following osmotic demyelination syndrome in a SARS-CoV-2 infected elderly diabetic woman: A case report. Neurologia (Engl Ed). 2022;37(8):706-8.
18. Ong TL, Nor KM, Yusoff Y, Sapuan S. COVID-19 Associated Acute Necrotizing Encephalopathy Presenting as Parkinsonism and Myorhythmia. J Mov Disord. 2022;15(1):89-92.
19. World Health Organization. Clinical management of severe acute respiratory infection when novel coronavirus (2019-nCoV) infection is suspected2020.
To cite this abstract in AMA style:
P. Polverino, S. Lalli, M. Lo Giudice, A. Albanese. Post-Covid parkinsonism: a systematic review of clinical presentations [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/post-covid-parkinsonism-a-systematic-review-of-clinical-presentations/. Accessed December 13, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/post-covid-parkinsonism-a-systematic-review-of-clinical-presentations/