Category: Parkinsonism, Others
Objective: To clinically characterize a cohort of patients with normal pressure hydrocephalus (NPH) to identify possible clinical and humoral biomarkers that can predict the response to the treatment.
Background: NPH is a late-onset neurological syndrome characterized by cerebral ventricles enlargement associated with motor, urinary, and cognitive symptoms that lead to serious disability such as gait disturbances, complete urinary incontinence, and severe dementia. NPH is a potentially reversible condition, that poses several diagnostic challenges, especially in the differential diagnosis with other movement disorders (i.e parkinsonism).
Method: 57 patients with a diagnosis of idiopathic NPH that underwent tap-test (TT) procedure were retrospectively enrolled at the Neurology Department of Policlinico Hospital in Milan from 2012 to 2021. Epidemiological, clinical, neuroradiological, neuropsychological, and cerebrospinal fluid (CSF) proteins data were collected, as well as clinical response to TT and ventriculoperitoneal shunt (VP).
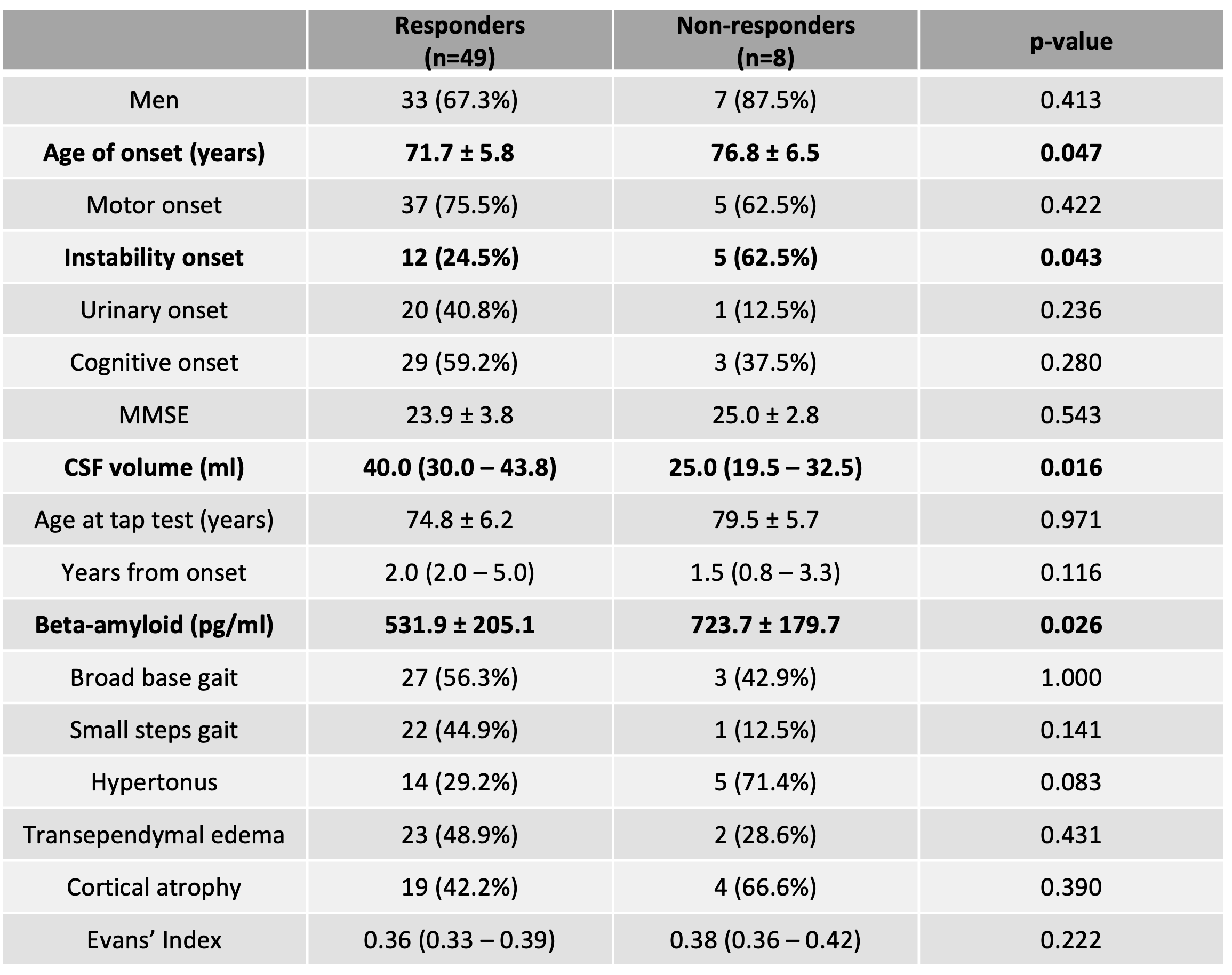
Results: The mean age of enrolled patients was 72,5 ± 6,6 years. 74% of them displayed motor symptoms at onset, 30% postural instability and falls, 37% urinary dysfunctions, and 56% cognitive impairment. Ventricular enlargement was observed in 98.2% of patients and Evans’ Index was > 0.3 in 86% of them. The median volume of collected CSF was 37.5 ml and 49 (86.0%) patients improved after TT (responders); the improvement was observed in motor (85%), urinary (20%), and cognitive function (38%). The mean CSF beta-amyloid level was 562.5 ± 211.6 pg/ml. 20 patients (35%) underwent VP surgery, and 89% of them showed an improvement in motor, 44% in urinary, and 46% in cognitive symptoms.
Responders showed an earlier age of onset compared to non-responders (71.7 vs 76.8 years, p=0.047), in addition to lower instability prevalence at onset (24.5 vs 62.5%, p=0.043), higher CSF collected volume (40 vs 25ml, p=0.016), and a lower CSF beta-amyloid value (531.9 vs 723.7 pg/ml, p=0.026). Patients who did not undergo VP shunt surgery showed lower scores at Mini-Mental State Examination (MMSE).
Conclusion: This study supports the evidence of a great clinical and therapeutical response heterogeneity and highlights some key aspects that may help clinicians during the diagnostic process, such as TT standardization, evaluation of CSF beta-amyloid levels, and alternative diagnoses exclusion.
To cite this abstract in AMA style:
A. Di Maio, G. Lazzeri, F. Arienti, F. Ruggiero, F. Mameli, A. Di Fonzo, G. Franco. Phenotypical and treatment response heterogeneity in a cohort of normal pressure hydrocephalus patients [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/phenotypical-and-treatment-response-heterogeneity-in-a-cohort-of-normal-pressure-hydrocephalus-patients/. Accessed February 13, 2026.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/phenotypical-and-treatment-response-heterogeneity-in-a-cohort-of-normal-pressure-hydrocephalus-patients/