Category: Parkinsonism, Others
Objective: To characterize the neutrophil-to-lymphocyte ratio (NLR) levels in the peripheral blood of patients with ventriculomegaly and its correlation with clinical outcomes
Background: Ventriculomegaly is the hallmark in patients with idiopathic normal pressure hydrocephalus (iNPH) and can be found in several neurodegenerative diseases such as Alzheimer’s disease (AD), Parkinson’s disease (PD), dementia with Lewy bodies (DCL), progressive supranuclear palsy (PSP). Elevated NLR in peripheral blood is common in these conditions. NLR assessment could aid clinicians in refining clinical management for patients with ventriculomegaly and associated neurodegenerative disorders
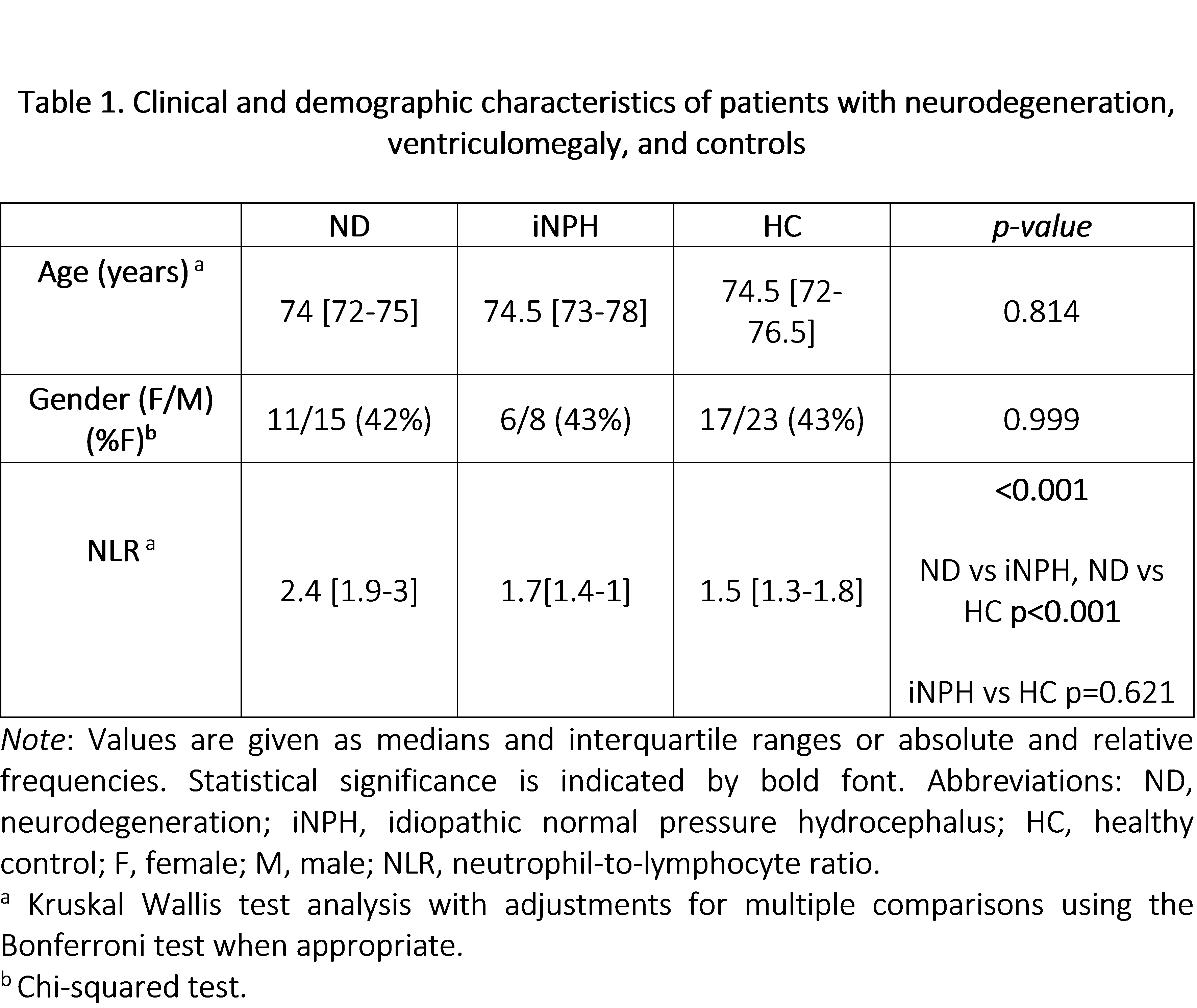
Method: A retrospective study at Clínica Universidad de Navarra’s Movement Disorders Unit involved 40 patients with ventriculomegaly and 40 controls [Table 1]. Brain MRI was conducted on all subjects. Ventriculomegaly was defined using the Evans Index (EI) and Callosal Angle (CA) thresholds (EI > 0.3 and CA < 100º).
Inflammatory markers including total white blood cell count and NLR were evaluated, with the exclusion of subjects prone to blood count alterations.
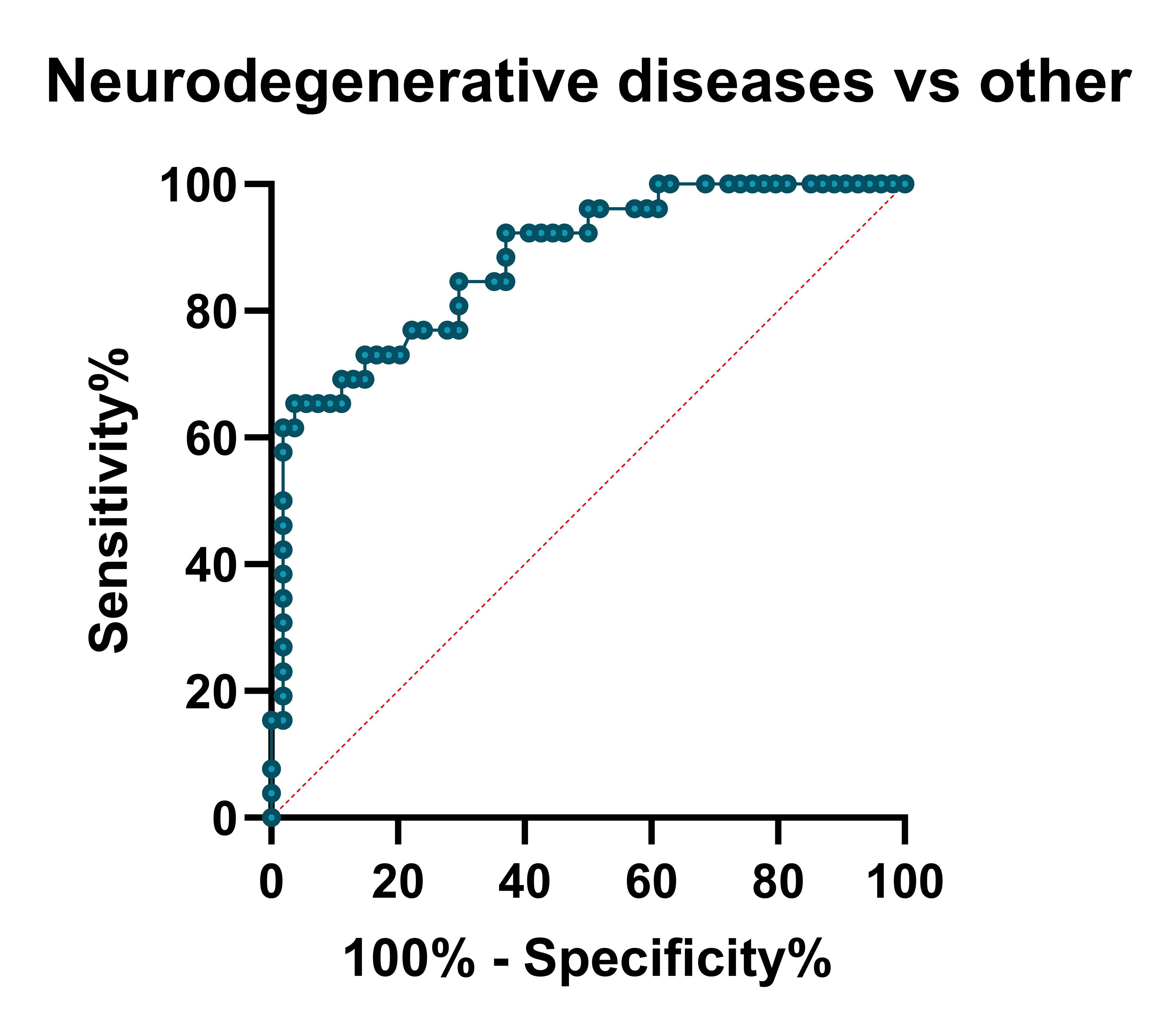
The Kruskal-Wallis test was used to assess differences among three NLR subgroups, with adjustments for multiple comparisons using the Bonferroni test. Categorical variables were analyzed with the chi-squared test. Receiver operating characteristic (ROC) curve analysis provided an area under the curve (AUC) and established NLR cutoffs [Figure 1].
Results: 50% (n=20) of patients with ventriculomegaly met clinical criteria for PSP, 12.5% (n=5) for AD, 2.5% (n=1) were diagnosed with DCL, and the remaining 35% of patients were diagnosed with iNPH. Patients with neurodegenerative conditions (PSP, AD, DCL) exhibited the highest NLR compared to iNPH and controls (2.4 [1.9-3] vs 1.7[1.4-1], p <0.001 vs 1.5 [1.3-1.8], p <0.001). However, NLR for iNPH compared to the control group reported (1.7 [1.4-1] vs 1.5 [1.3-1.8] p=0.62) [Table 1]. The ROC analysis provided an AUC for NLR, at the given cutoff value >2.0, NLR differentiated neurodegeneration versus other patients with a sensitivity of 73% and a specificity of 85%.
Conclusion: Our results suggest that in patients with ventriculomegaly, the NLR could be a potential biomarker for differentiating neurogenerative diseases from those with iNPH
Table 1
Figure 1. Cutoff values
References: 1. Bissacco J, Simonetta C, Mascioli D, Zenuni H, Bovenzi R, Grillo P, Di Giuliano F, Stefani A, Mercuri NB, Schirinzi T. Peripheral immunity changes are associated with neurodegeneration and worse clinical outcome in idiopathic normal pressure hydrocephalus. Eur J Neurol. 2024 Mar;31(3):e16179. doi: 10.1111/ene.16179. Epub 2023 Dec 21. PMID: 38130035.
2. Espay AJ, Da Prat GA, Dwivedi AK, Rodriguez-Porcel F, Vaughan JE, Rosso M, Devoto JL, Duker AP, Masellis M, Smith CD, Mandybur GT, Merola A, Lang AE. Deconstructing normal pressure hydrocephalus: Ventriculomegaly as early sign of neurodegeneration. Ann Neurol. 2017 Oct;82(4):503-513. doi: 10.1002/ana.25046. Epub 2017 Oct 4. PMID: 28892572.
3. Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM. Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery. 2005 Sep;57(3 Suppl):S4-16; discussion ii-v. doi: 10.1227/01.neu.0000168185.29659.c5. PMID: 16160425.
To cite this abstract in AMA style:
C. Espinoza-Vinces, I. Avilés-Olmos, G. Martí-Andrés, M. Jiménez-Vázquez, M. Calvo-Imirizaldu, M. Marín Gracia, R. Villino-Rodríguez, A. Atorrasagasti-Villar, J. Arbizu, MR. Luquin. Peripheral immunity and clinical phenotypes in patients with ventriculomegaly [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/peripheral-immunity-and-clinical-phenotypes-in-patients-with-ventriculomegaly/. Accessed April 18, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/peripheral-immunity-and-clinical-phenotypes-in-patients-with-ventriculomegaly/