Category: Parkinson's Disease: Non-Motor Symptoms
Objective: The primary outcome was assessing QoL of a cohort of patients with PD before and after undergoing DBS surgery, measured using PDQ-39 questionary. Secondary outcomes included motor symptoms according to UPDRS-III scale and metabolic effects assessed by body mass index (BMI) and waist circumference.
Background: Deep brain stimulation (DBS) is a treatment indicated in selected patients with Parkinson’s disease (PD), in whom motor fluctuations and dyskinesias predominate and in patients with poor response to best medical treatment (BMT). The identification of predictors of improvement in Quality of life (QoL) after surgery is fundamental in the selection of candidates for DBS.
Method: A prospective observational study was conducted in a tertiary hospital to compare neurostimulation plus medical therapy (DBS group) with best medical treatment alone (BMT group) in patients with PD.
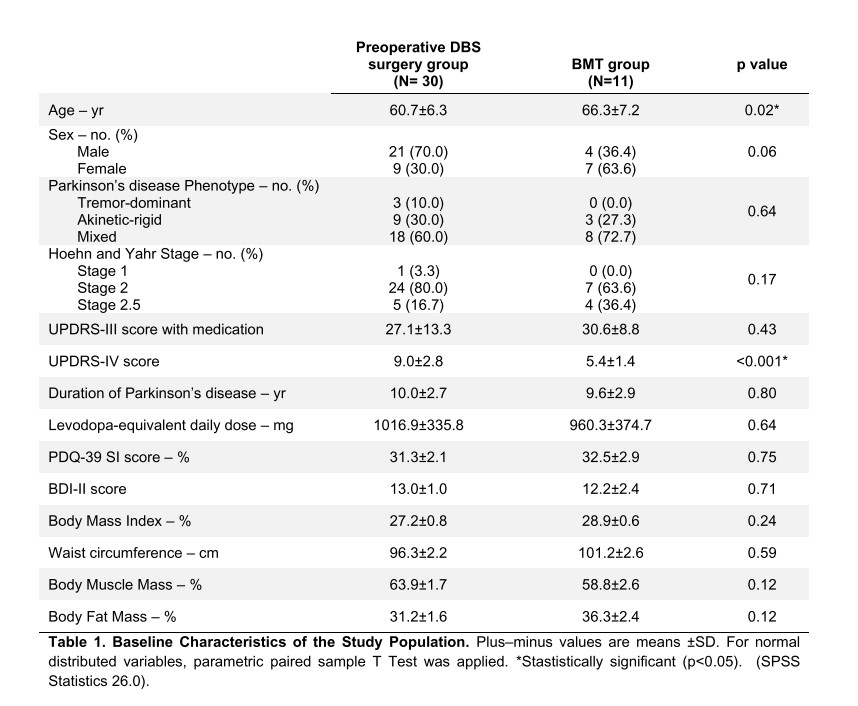
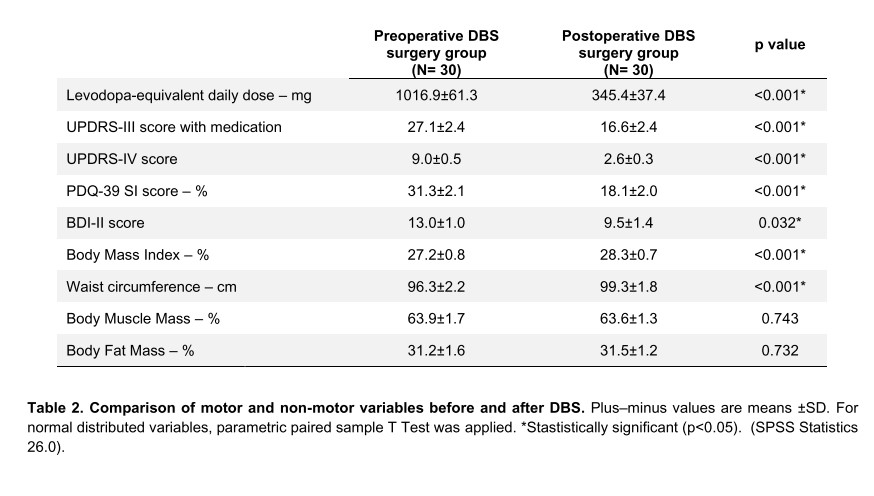
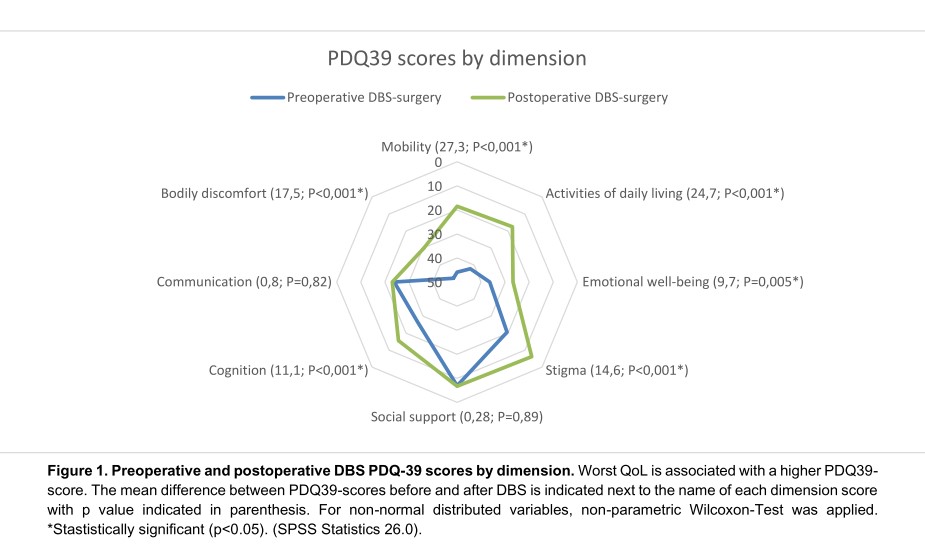
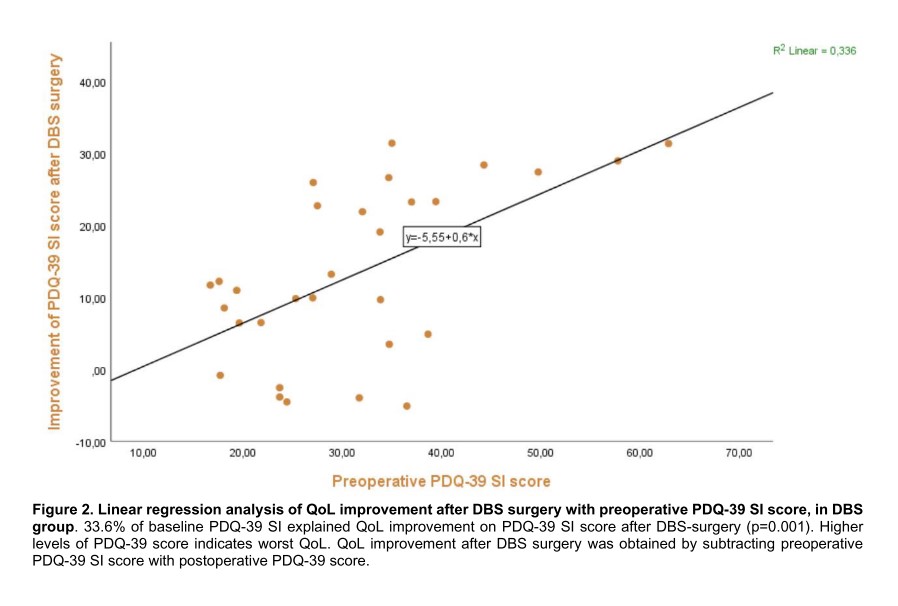
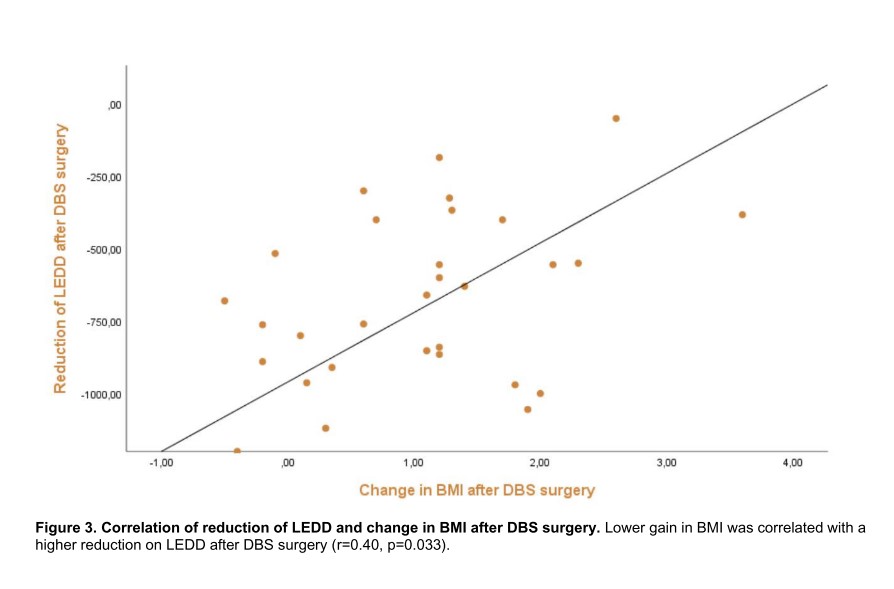
Results: A total of 41 patients with PD were enrolled between 2021 and 2023: 30 patients underwent DBS surgery and 11 patients were treated with BMT alone. Participants were revaluated between 6 to 12 months after surgery. PDQ-39 SI score had a mean improvement of 42.3% in the DBS group after surgery (p<0,001). After surgery the DBS group had a mean difference of 44.5% in the PDQ-39 SI score compared to the BMT group (p<0.001). After executing a linear regression model, baseline PDQ-39 SI score explains 33.6% of QoL improvement after DBS surgery (p=0.001). No association was found between QoL and other clinical characteristics. UPDRS-III had a mean improvement of 38.7% in the DBS group after surgery, and had an improvement of 45.7% compared to the BMT group (p<0.001). There was an increase in BMI of 1.05% and 3.0 cm on waist circumference after surgery (p<0.001). No association was found between metabolic effects and the improvement of motor or QoL after surgery.
Conclusion: Preoperative PDQ-39 SI scores could be useful to guide the selection of patients for DBS surgery. Adverse effects related to DBS surgery such as metabolic features should be considered in the decision.
References: 1. Bloem BR, Okun MS, Klein C. Parkinson’s disease. Lancet 2021;397(10291):2284-2303. (In eng). DOI: 10.1016/s0140-6736(21)00218-x.
2. Zhao N, Yang Y, Zhang L, et al. Quality of life in Parkinson’s disease: A systematic review and meta-analysis of comparative studies. CNS Neurosci Ther 2021;27(3):270-279. (In eng). DOI: 10.1111/cns.13549.
3. Mansouri A, Taslimi S, Badhiwala JH, et al. Deep brain stimulation for Parkinson’s disease: meta-analysis of results of randomized trials at varying lengths of follow-up. J Neurosurg 2018;128(4):1199-1213. (In eng). DOI: 10.3171/2016.11.Jns16715.
4. Rughani A, Schwalb JM, Sidiropoulos C, et al. Congress of Neurological Surgeons Systematic Review and Evidence-Based Guideline on Subthalamic Nucleus and Globus Pallidus Internus Deep Brain Stimulation for the Treatment of Patients With Parkinson’s Disease: Executive Summary. Neurosurgery 2018;82(6):753-756. (In eng). DOI: 10.1093/neuros/nyy037.
5. Pollak P. Deep brain stimulation for Parkinson’s disease – patient selection. Handb Clin Neurol 2013;116:97-105. (In eng). DOI: 10.1016/b978-0-444-53497-2.00009-7.
6. Goetz CG, Tilley BC, Shaftman SR, et al. Movement Disorder Society-sponsored revision of the Unified Parkinson’s Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Mov Disord 2008;23(15):2129-70. (In eng). DOI: 10.1002/mds.22340.
7. Fox SH, Katzenschlager R, Lim SY, et al. International Parkinson and movement disorder society evidence-based medicine review: Update on treatments for the motor symptoms of Parkinson’s disease. Mov Disord 2018;33(8):1248-1266. (In eng). DOI: 10.1002/mds.27372.
8. Frizon LA, Hogue O, Achey R, et al. Quality of Life Improvement Following Deep Brain Stimulation for Parkinson Disease: Development of a Prognostic Model. Neurosurgery 2019;85(3):343-349. (In eng). DOI: 10.1093/neuros/nyy287.
9. Peng L, Fu J, Ming Y, Zeng S, He H, Chen L. The long-term efficacy of STN vs GPi deep brain stimulation for Parkinson disease: A meta-analysis. Medicine (Baltimore) 2018;97(35):e12153. (In eng). DOI: 10.1097/md.0000000000012153.
10. Krause P, Reimer J, Kaplan J, et al. Deep brain stimulation in Early Onset Parkinson’s disease. Front Neurol 2022;13:1041449. (In eng). DOI: 10.3389/fneur.2022.1041449.
11. Schuepbach WM, Rau J, Knudsen K, et al. Neurostimulation for Parkinson’s disease with early motor complications. N Engl J Med 2013;368(7):610-22. (In eng). DOI: 10.1056/NEJMoa1205158.
12. Geraedts VJ, Feleus S, Marinus J, van Hilten JJ, Contarino MF. What predicts quality of life after subthalamic deep brain stimulation in Parkinson’s disease? A systematic review. Eur J Neurol 2020;27(3):419-428. (In eng). DOI: 10.1111/ene.14147.
13. Huang LC, Chen LG, Wu PA, et al. Effect of deep brain stimulation on brain network and white matter integrity in Parkinson’s disease. CNS Neurosci Ther 2022;28(1):92-104. (In eng). DOI: 10.1111/cns.13741.
14. Samborska-Ćwik J, Szlufik S, Friedman A, Mandat T, Przybyszewski A, Koziorowski D. Influence of Bilateral Subthalamic Nucleus Deep Brain Stimulation on the Lipid Profile in Patients With Parkinson’s Disease. Front Neurol 2020;11:563445. (In eng). DOI: 10.3389/fneur.2020.563445.
15. Monteferrante NR, Wilhelmi BG, Lambert M, Ponce FA. Effects of implantation of a deep brain stimulation device on patient weight in Parkinson’s disease and essential tremor. J Neurosurg 2020;134(5):1624-1630. (In eng). DOI: 10.3171/2020.2.Jns192354.
16. Steinhardt J, Münte TF, Schmid SM, Wilms B, Brüggemann N. A systematic review of body mass gain after deep brain stimulation of the subthalamic nucleus in patients with Parkinson’s disease. Obes Rev 2020;21(2):e12955. (In eng). DOI: 10.1111/obr.12955.
17. Vieira E. Qualidade de vida na doença de Parkinson. [Dissertação de Mestrado]. Coimbra: Faculdade de Medicina da Universidade de Coimbra2008.
18. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. Jama 2013;310(20):2191-4. (In eng). DOI: 10.1001/jama.2013.281053.19. Defer GL, Widner H, Marié RM, Rémy P, Levivier M. Core assessment program for surgical interventional therapies in Parkinson’s disease (CAPSIT-PD). Mov Disord 1999;14(4):572-84. (In eng). DOI: 10.1002/1531-8257(199907)14:4<572::aid-mds1005>3.0.co;2-c.
20. Postuma RB, Berg D, Stern M, et al. MDS clinical diagnostic criteria for Parkinson’s disease. Mov Disord 2015;30(12):1591-601. (In eng). DOI: 10.1002/mds.26424.
21. Picillo M, Lozano AM, Kou N, Puppi Munhoz R, Fasano A. Programming Deep Brain Stimulation for Parkinson’s Disease: The Toronto Western Hospital Algorithms. Brain Stimul 2016;9(3):425437. (In eng). DOI: 10.1016/j.brs.2016.02.004.
22. Ferreira JJ, Katzenschlager R, Bloem BR, et al. Summary of the recommendations of the EFNS/MDS-ES review on therapeutic management of Parkinson’s disease. Eur J Neurol 2013;20(1):5-15. (In eng). DOI: 10.1111/j.1468-1331.2012.03866.x.
23. Campos RC, & Gonçalves, B. , 25 a 27 de Julho. . Adaptação do Inventário de Depressão de Beck II para a população portuguesa. Actas do VIII Congresso Iberoamericano de Avaliação Psicológica. Lisboa2011.
24. Hariz M, Blomstedt P. Deep brain stimulation for Parkinson’s disease. J Intern Med 2022;292(5):764-778. (In eng). DOI: 10.1111/joim.13541.
25. Lange F, Eldebakey H, Hilgenberg A, et al. Distinct phenotypes of stimulation-induced dysarthria represent different cortical networks in STN-DBS. Parkinsonism Relat Disord 2023;109:105347. (In eng). DOI: 10.1016/j.parkreldis.2023.105347.
26. Spagna S, Askari A, Wyant KJ, et al. Perceived social support declines after deep brain stimulation surgery in patients with Parkinson’s disease. J Neural Transm (Vienna) 2022;129(12):1463-1468. (In eng). DOI: 10.1007/s00702-022-02558-6.
27. Schuepbach WMM, Tonder L, Schnitzler A, et al. Quality of life predicts outcome of deep brain stimulation in early Parkinson disease. Neurology 2019;92(10):e1109-e1120. (In eng). DOI: 10.1212/wnl.0000000000007037.
28. Abboud H, Genc G, Thompson NR, et al. Predictors of Functional and Quality of Life Outcomes following Deep Brain Stimulation Surgery in Parkinson’s Disease Patients: Disease, Patient, and Surgical Factors. Parkinsons Dis 2017;2017:5609163. (In eng). DOI: 10.1155/2017/5609163.
To cite this abstract in AMA style:
L. Torrão, M. Rosas, J. Massano, A. Oliveira, C. Chamadoira, M. Rito, J. Guimarães, C. Soares. PDQ-39 predicts quality of life improvement following neurostimulation for Parkinson’s disease: Prospective observational study [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/pdq-39-predicts-quality-of-life-improvement-following-neurostimulation-for-parkinsons-disease-prospective-observational-study/. Accessed April 26, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/pdq-39-predicts-quality-of-life-improvement-following-neurostimulation-for-parkinsons-disease-prospective-observational-study/