Objective: Two studies were conducted to compare the safety, effectiveness, and comfort of fixed- and variable-frequency transcutaneous afferent patterned stimulation (TAPS) for action tremor relief in essential tremor (ET) and Parkinson’s disease (PD).
Background: TAPS of the median and radial nerves at the wrist is calibrated to patients’ tremor frequency and was shown to improve symptoms of ET [1]. Adding burst or pulse frequency variation (BFV, PFV) over time in the TAPS pattern may better align therapy with natural variations in tremor frequency [2] and improve symptom relief.
Method: Two prospective, double-blinded studies enrolled 30 and 15 patients with ET and PD, respectively. Patients performed 2 weeks each of TAPS with (1) standard, fixed frequency (FF), (2) BFV of ±1.6 Hz around their tremor frequency, and (3) PFV between 50-150 Hz on their dominant hand in a random order. Each 2-week period included a clinical assessment visit and a home-use period where patients performed two therapy sessions daily. Primary effectiveness endpoints were tremor power improvement ratio (TPIR=powerpre/powerpost) as measured via accelerometer during postural hold, and changes in Bain & Findley Activities of Daily Living (ADL) assessed from pre- to post-stimulation. Comfort was evaluated by patient survey (5-point scale), and safety was assessed by adverse events (AE).
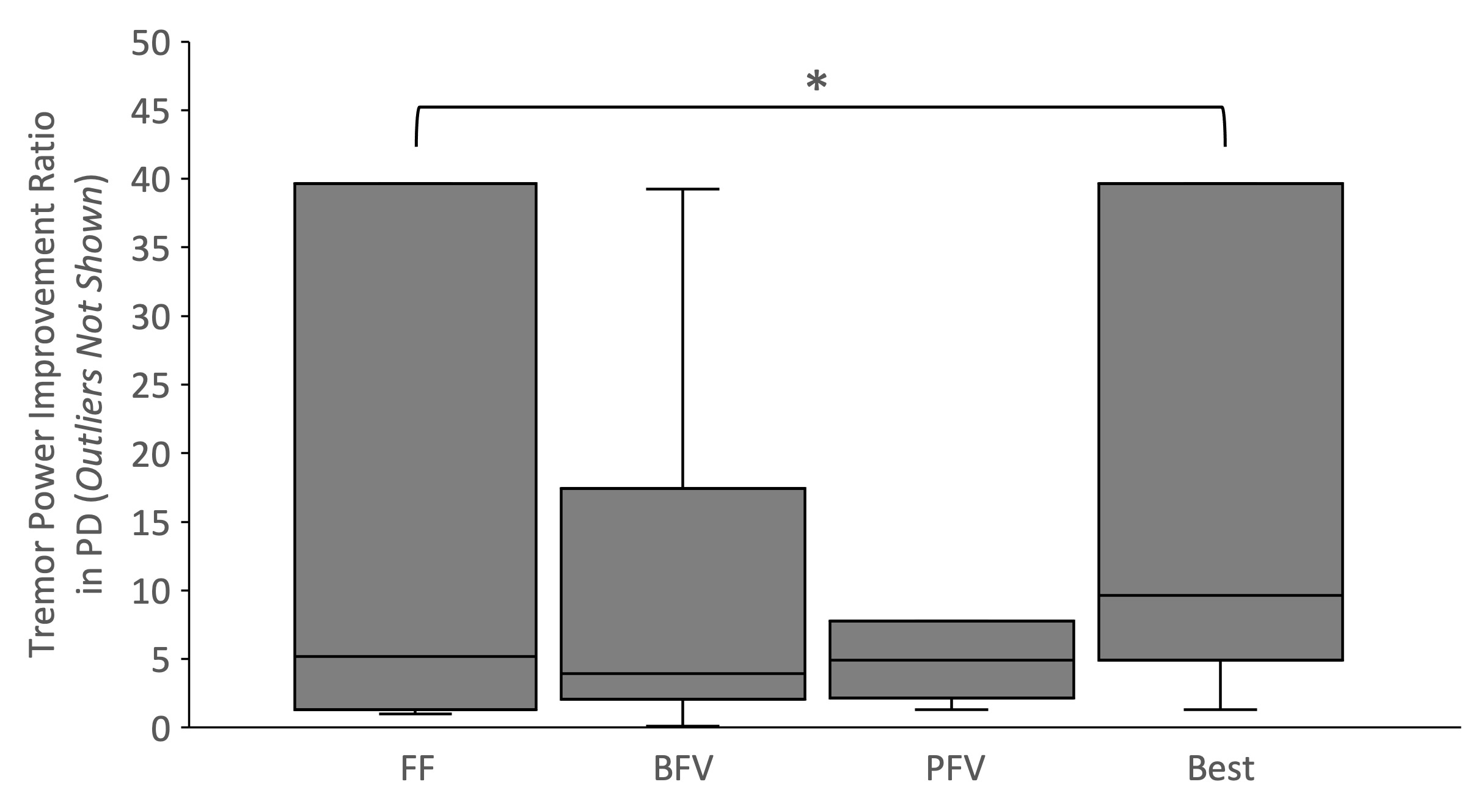
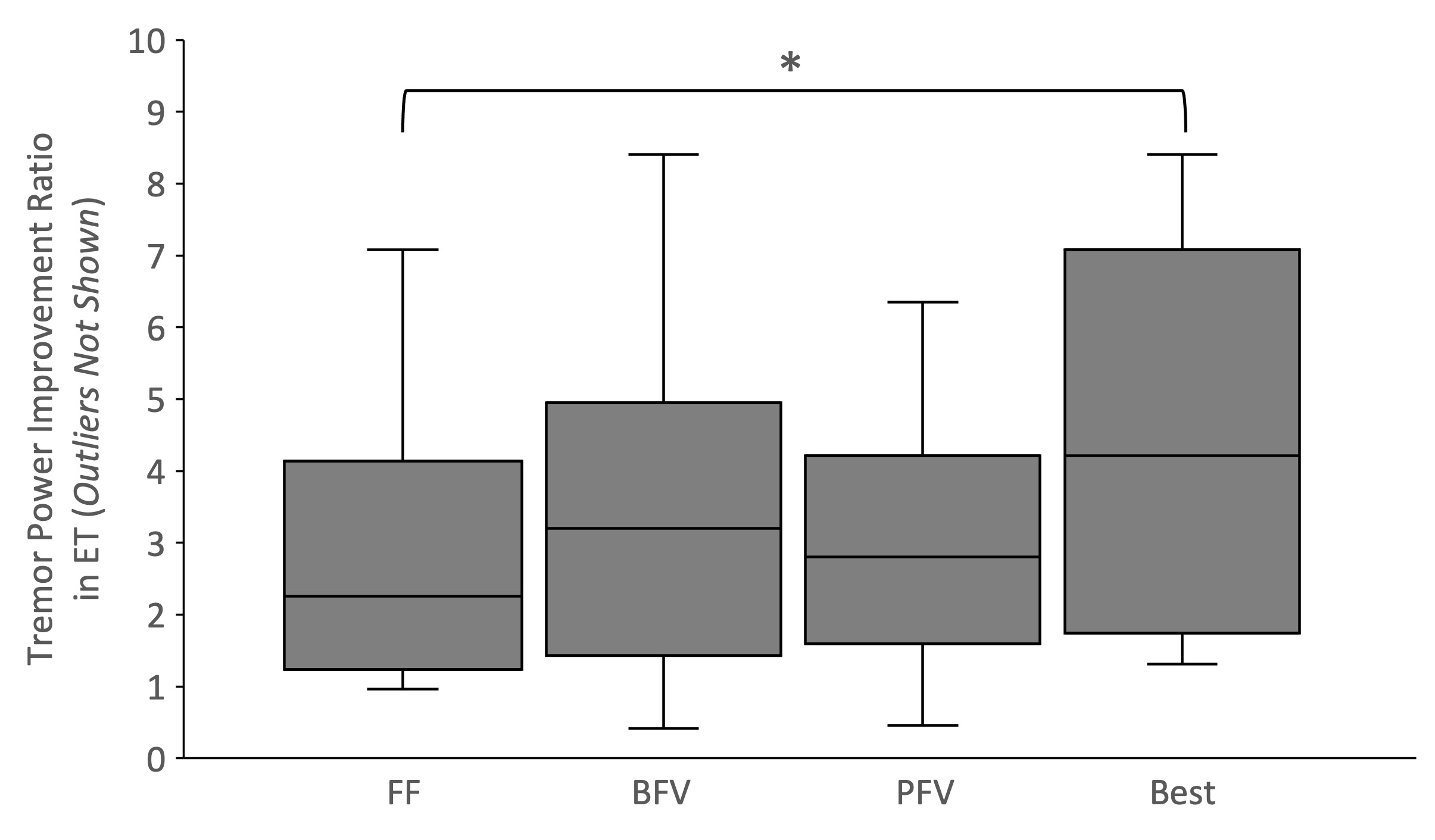
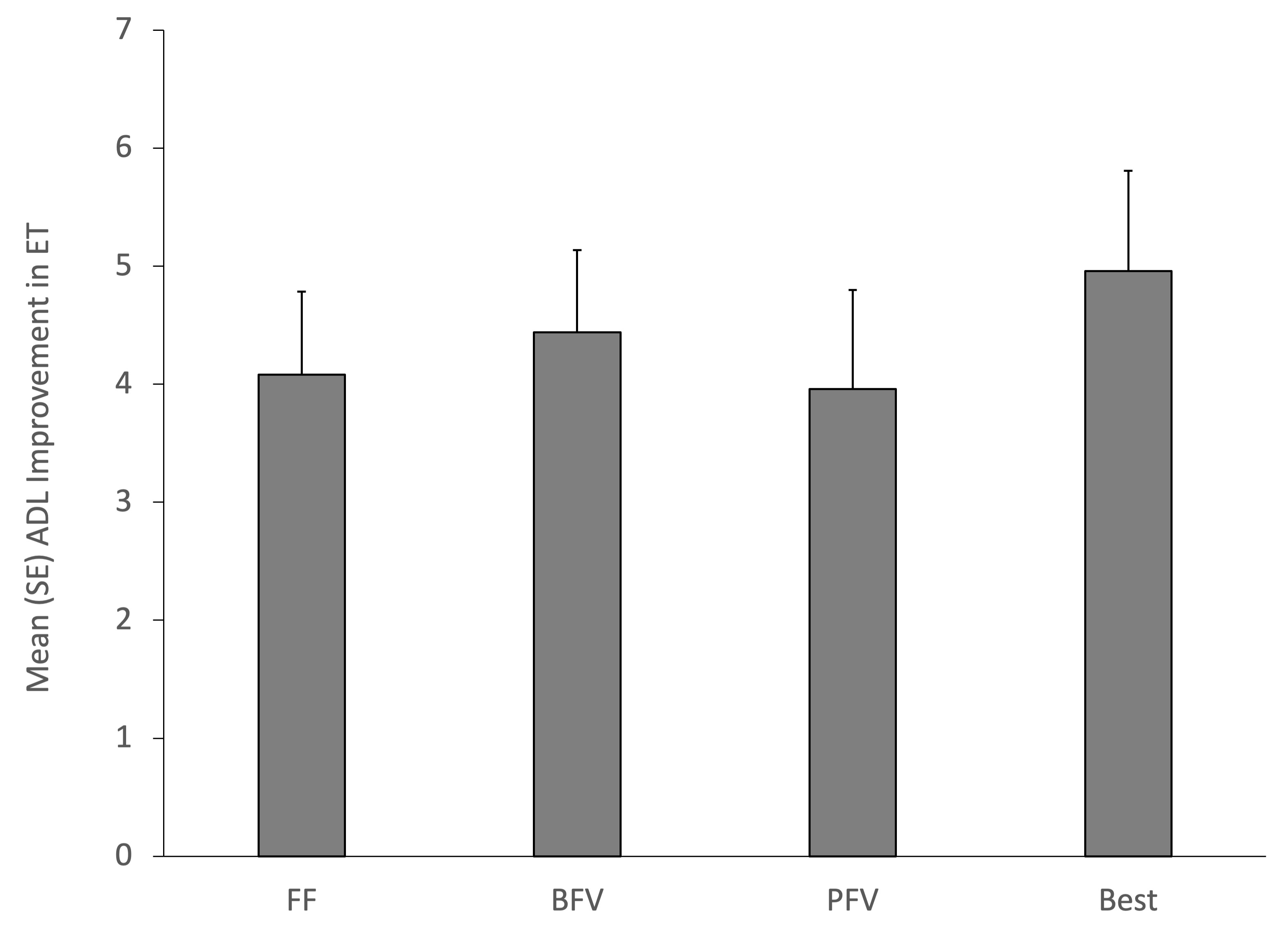
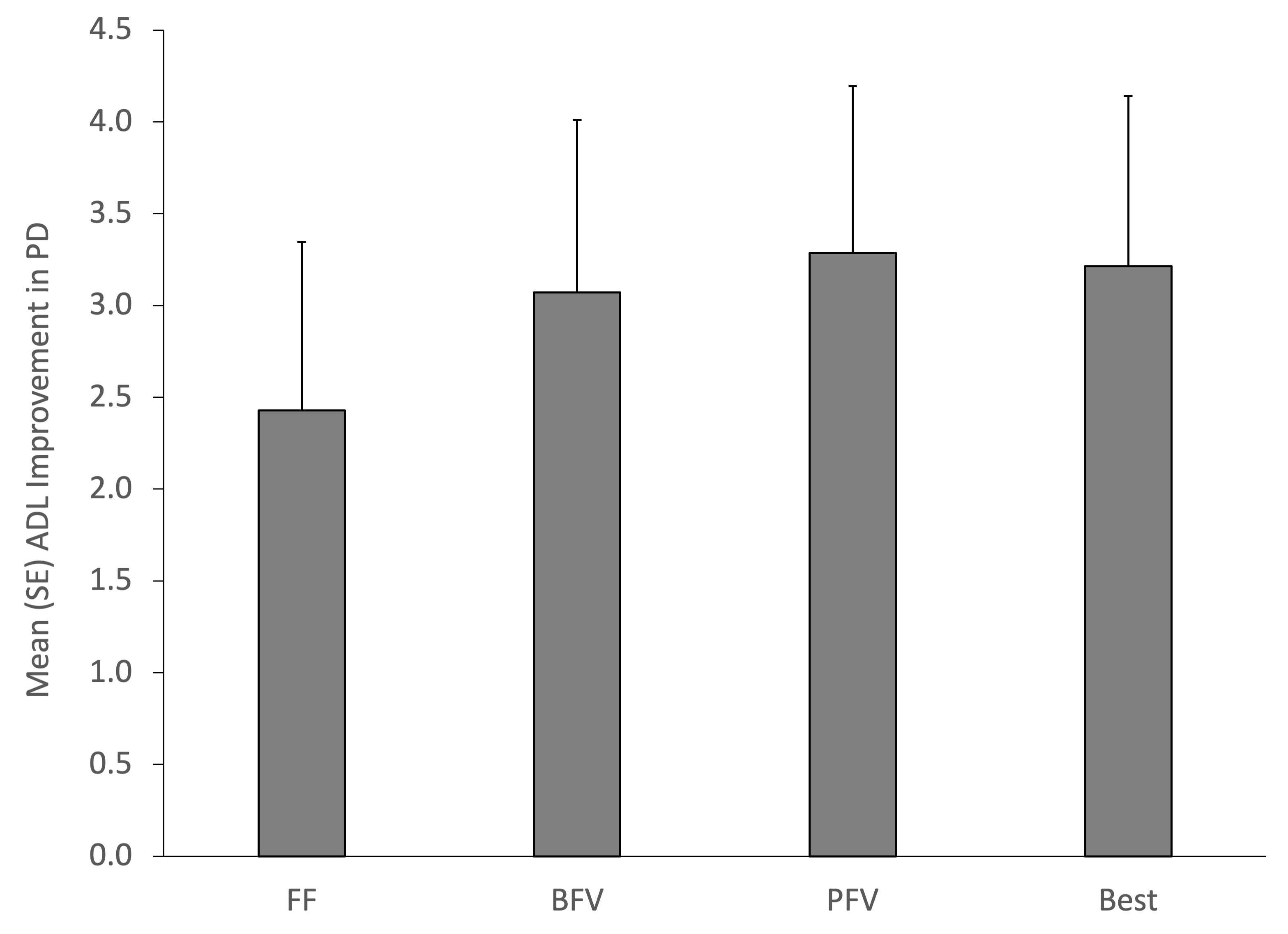
Results: Adding frequency variation to TAPS did not improve population-level outcomes for median TPIR (ET: 2.3, 3.2, 2.8 for FF, BFV, PFV, p=0.29; PD: 5.2, 3.9, 4.9, p=0.93) or mean ADL improvement (ET: 4.1, 4.4, 4.0, p=0.75; PD: 2.4, 3.1, 3.3, p=0.42). Selecting patient-specific best TAPS patterns, based on TPIR, significantly increased median TPIR by 86% in both ET and PD (p<0.0001), and increased mean ADL improvement by 22% in ET and 32% in PD (p=0.15, ns).
Variable-frequency TAPS may have improved comfort in PD (3.5, 4.1, 3.8, p=0.06), but was similar in ET (3.1, 3.1, 3.0, p=0.87). Patient-specific best TAPS pattern did not improve comfort (ET: -1% change, p=0.81; PD: 10%, p=0.25).
Twenty-two AEs were reported, with skin irritation being most common; there were no differences in AE rates across patterns (p>0.45).
Conclusion: These studies demonstrate that recommending the best TAPS pattern for each patient with ET and PD, based on their measured response to each pattern, improves therapeutic outcomes.
References: 1. Isaacson, S.H. et al. Prospective home-use study on non-invasive neuromodulation therapy for essential tremor. Tremor Other Hyperkinet Mov, 2020; 10: 29.
2. O’Suilleabhain, P.E. and Matsumoto J.Y. Time-frequency analysis of tremors. Brain, 1998; 121: 2127-34.
To cite this abstract in AMA style:
A. Kent, H. Kim, D. Khosla, K. Rosenbluth. Patient-Specific Outcomes of Transcutaneous Afferent Patterned Stimulation with Varying Frequencies for Essential Tremor and Parkinson’s Disease [abstract]. Mov Disord. 2022; 37 (suppl 2). https://www.mdsabstracts.org/abstract/patient-specific-outcomes-of-transcutaneous-afferent-patterned-stimulation-with-varying-frequencies-for-essential-tremor-and-parkinsons-disease/. Accessed January 30, 2026.« Back to 2022 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/patient-specific-outcomes-of-transcutaneous-afferent-patterned-stimulation-with-varying-frequencies-for-essential-tremor-and-parkinsons-disease/