Session Information
Date: Tuesday, September 24, 2019
Session Title: Parkinsonisms and Parkinson-Plus
Session Time: 1:45pm-3:15pm
Location: Agora 3 West, Level 3
Objective: Present an original case description of a patient with amebic meningoencephalitis.
Background: Parkinsonism could be caused by degenerative disorders, brain injuries, drugs, toxins, and infections. Free-living amoebas (FLA) exist in nature without the need for a host; Naegleria, Acanthamoeba, Balamuthia, and Sappinia cause CNS infection with two clinical syndromes well recognized: Primary and granulomatous amebic encephalitis. These are rare causes of CNS infection which must be considered in patients with no response to antibiotic treatment and exposition risk. FLA are widely found in the American continent. Hispanic patients are possible more affected; it has been correlated with agricultural exposure, swimming or gardening. A literature search was done at Pubmed, Scopus, and Web of Science. We did not find reports of parkinsonism and FLA until now.
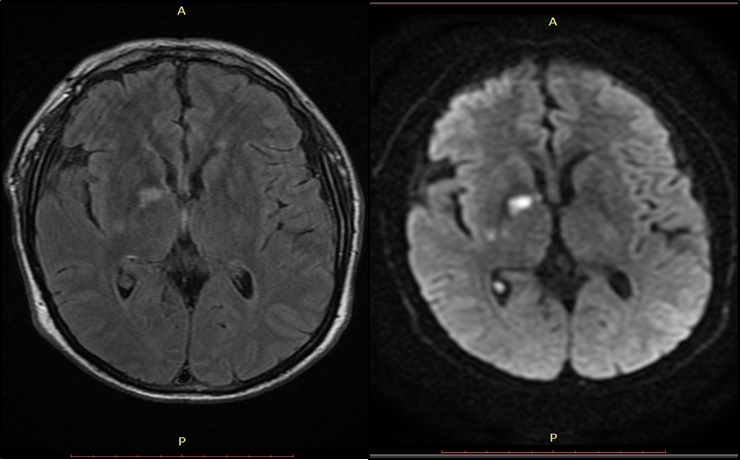
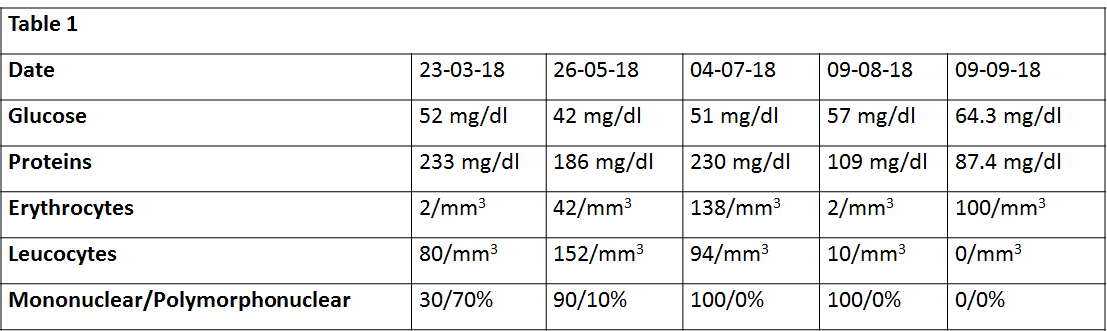
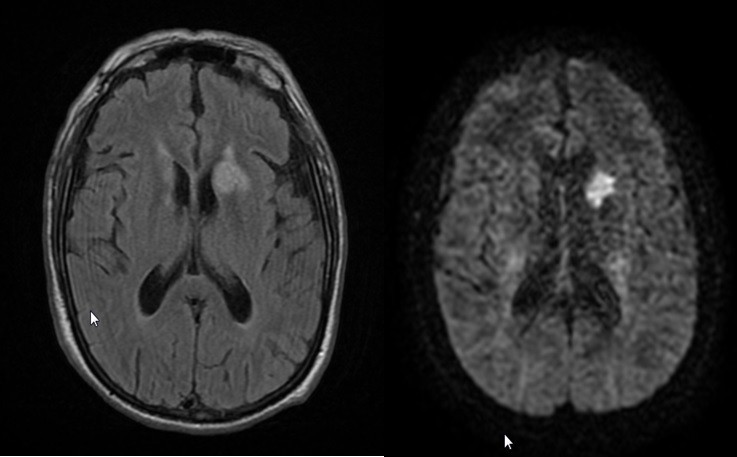
Method: A 60-year old man with hypertension and DM2. Onset: March 2018 with diarrhea, abdominal pain, fever, nausea, and a non-ulcerated plaque diagnosed as herpes in the right thigh. He received symptomatic treatment at the ER. Ten days later, tonic-clonic seizures, fever, disorientation, and gait instability. EEG: Left temporal and frontal epileptic discharges; MRI: right striatal lesion [figure1], LP [Table1]. Meningeal tuberculosis treatment was initiated without improvement. Two months later, he presented impaired mentation, shuffling steps, bradykinesia, tremor, insomnia, and loss control of sphincters. Another LP was done (Table1]; a new MRI showed a different left striatum lesion [Figure2]. Levodopa, citalopram, and prednisone were added to tuberculosis treatment: Clinical and control LP two weeks later [Table1] without improvement.
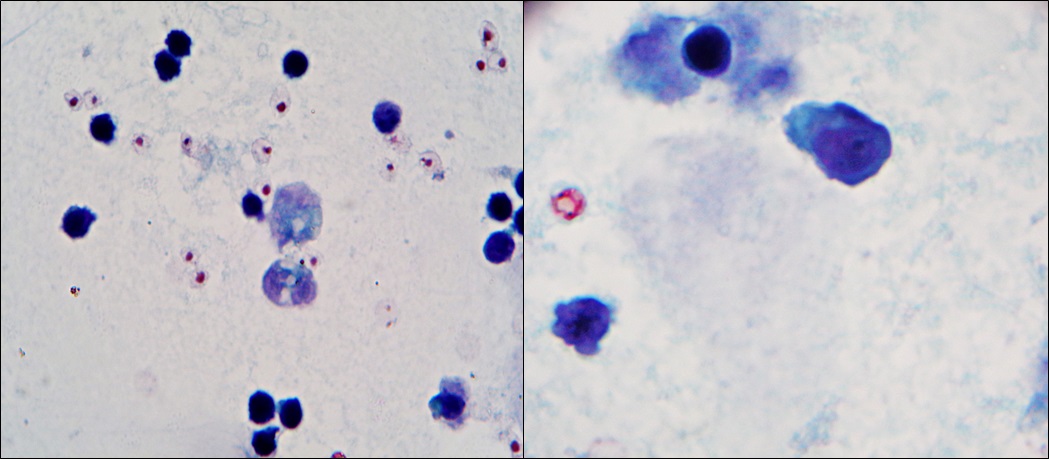
Results: Meningeal biopsy and cerebrospinal fluid cytology: Presence of a free-living amoeba [Figure3]. Treatment with Amphotericin-B, chloramphenicol, albendazole, trimethoprim-sulfamethoxazole, and rifampicin was prescribed with a progressive and dramatic clinical improvement (cognition, language, tremor, and speed of gait) and in subsequent CSF samples [Table1].
Conclusion: : To our knowledge, there are no previous reports of the association between parkinsonism and CNS free-living ameba infection. Epidemiology, histopathologic examination, and treatment response let us recognize an FLA different of Naegleria, Balamuthia or Acanthamoeba as the causal agent for this uncommon disorder.
References: 1. Schuster FL, Visvesvara GS. Free-living amoebae as opportunistic and non-opportunistic pathogens of humans and animals. International Journal for Parasitology. 2004 Aug;34(9):1001–27. 2. Trabelsi H, Dendana F, Sellami A, Sellami H, Cheikhrouhou F, Neji S, et al. Pathogenic free-living amoebae: Epidemiology and clinical review. Pathologie Biologie. 2012 Dec;60(6):399–405. 3. Visvesvara GS. Infections with free-living amebae. In: Handbook of Clinical Neurology [Internet]. Elsevier; 2013 p. 153–68. 4. Campos P, Cabrera J, Gotuzzo E, Guillén D. Neurological involvement in free living amebiasis. Rev Neurol. 1999 Aug 16;29(4):316–8. 5. Król-Turmińska K, Olender A. Human infections caused by free-living amoebae. Annals of Agricultural and Environmental Medicine [Internet]. 2017 Mar 1.
To cite this abstract in AMA style:
M. Rubio Hernandez, I. Rodriguez Leyva, M. Tello Zavala, A. Ortiz Alvarez, C. Gallegos Rios. Parkinsonism and rapidly progressive dementia secondary to free-living ameba [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/parkinsonism-and-rapidly-progressive-dementia-secondary-to-free-living-ameba/. Accessed December 22, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/parkinsonism-and-rapidly-progressive-dementia-secondary-to-free-living-ameba/