Category: Parkinson's Disease: Non-Motor Symptoms
Objective: We aimed to identify whether orthostatic hypotension (OH) is a prodromal marker of Parkinson’s disease (PD) or a symptom of later disease.
Background: Many patients with PD experience OH symptoms during the course of their illness. Although OH has long been attributed to a more advanced stage of the disease, more recently studies suggested that OH is a prodromal marker of PD. However, these studies were performed in highly selected patient populations or were registry-based studies with different definitions of OH. The association between OH and PD in the general population has been limitedly studied so far.
Method: This study was embedded in the Rotterdam Study, a large prospective population-based cohort study in the Netherlands. We measured early OH (<1 minute), OH (<3 minutes), delayed OH (<5 minutes), symptomatic OH and neurogenic OH in 6,600 participants between 1989 and 1993. First, we determined the relation between prevalent PD and OH using logistic regression. Second, we followed PD-free participants for the occurrence of PD until January 1st, 2016 and studied the association between OH and the risk of PD using Cox proportional-hazards models. All models were adjusted for age and sex.
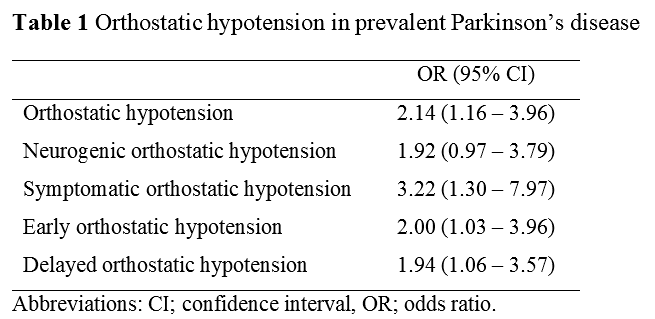
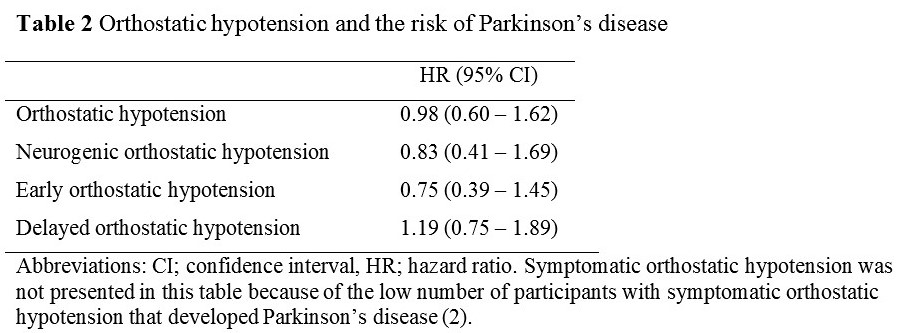
Results: The mean age (SD) of the study population was 69.1 (8.9) years and 59.3% were women. OH was present in 1,269 (19.9%) participants and 51 (0.8%) had PD at the time of OH measurement. Presence of PD was significantly associated with OH, symptomatic OH and both early and delayed OH (Table 1). The strongest association was found for symptomatic OH (OR 3.22, 95% CI: 1.30-7.97). Neurogenic OH was also associated with PD, although this association was not significant (OR 1.92, 95% CI: 0.97-3.79). After exclusion of participants with prevalent PD or without consent for follow-up, 6,053 individuals remained for the longitudinal analysis. During a mean follow-up of 14.6 years (7.6), 111 participants were diagnosed with incident PD. OH at baseline was not associated with an increased risk of PD (HR 0.98, 95% CI: 0.60-1.62) (Table 2). In addition, we found no association between neurogenic OH, early OH or delayed OH and the risk of PD.
Conclusion: We found an association between prevalent PD and OH, but we did not find an association between OH and the risk of PD. Our current data do not support the notion that OH is a prodromal marker of PD. Future population-based studies are warranted to replicate our findings.
[table1]
[table2]
To cite this abstract in AMA style:
L. Dommershuijsen, A. Heshmatollah, P. Koudstaal, M. Ikram, M. Ikram. Orthostatic hypotension in Parkinson’s disease [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/orthostatic-hypotension-in-parkinsons-disease/. Accessed December 23, 2025.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/orthostatic-hypotension-in-parkinsons-disease/