Category: Parkinson's Disease: Non-Motor Symptoms
Objective: To explore correlations between the identification status of individual odors in the Pennsylvania Smell Identification Test (UPSIT) and the clinical severity of Parkinson’s disease (PD).
Background: Olfactory dysfunction is the most common non-motor symptom in PD [1]. Limited research has discussed the relationship between the identification status of individual odors and PD clinical symptoms.
Method: PD patients were recruited from Taichung Veterans General Hospital between October 2016 and April 2022. Demographic information and clinical assessments, including UPSIT and other questionnaires, were collected during the on-medication status. Logistic regression analysis, incorporating age, gender, and levodopa equivalent daily dose (LEDD) as covariates, was conducted to explore the correlation between the misidentification of individual odors in the UPSIT and the severity of PD symptoms.
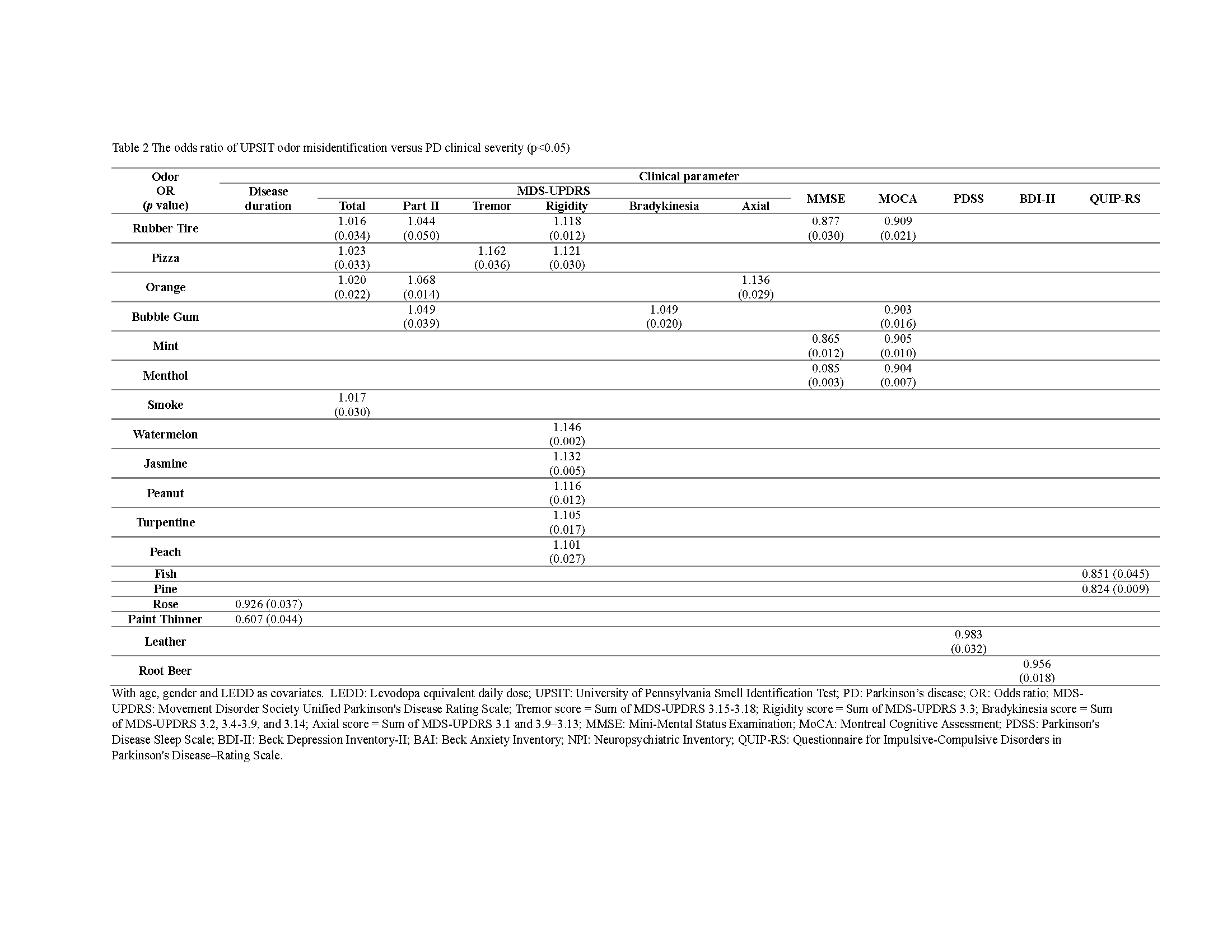
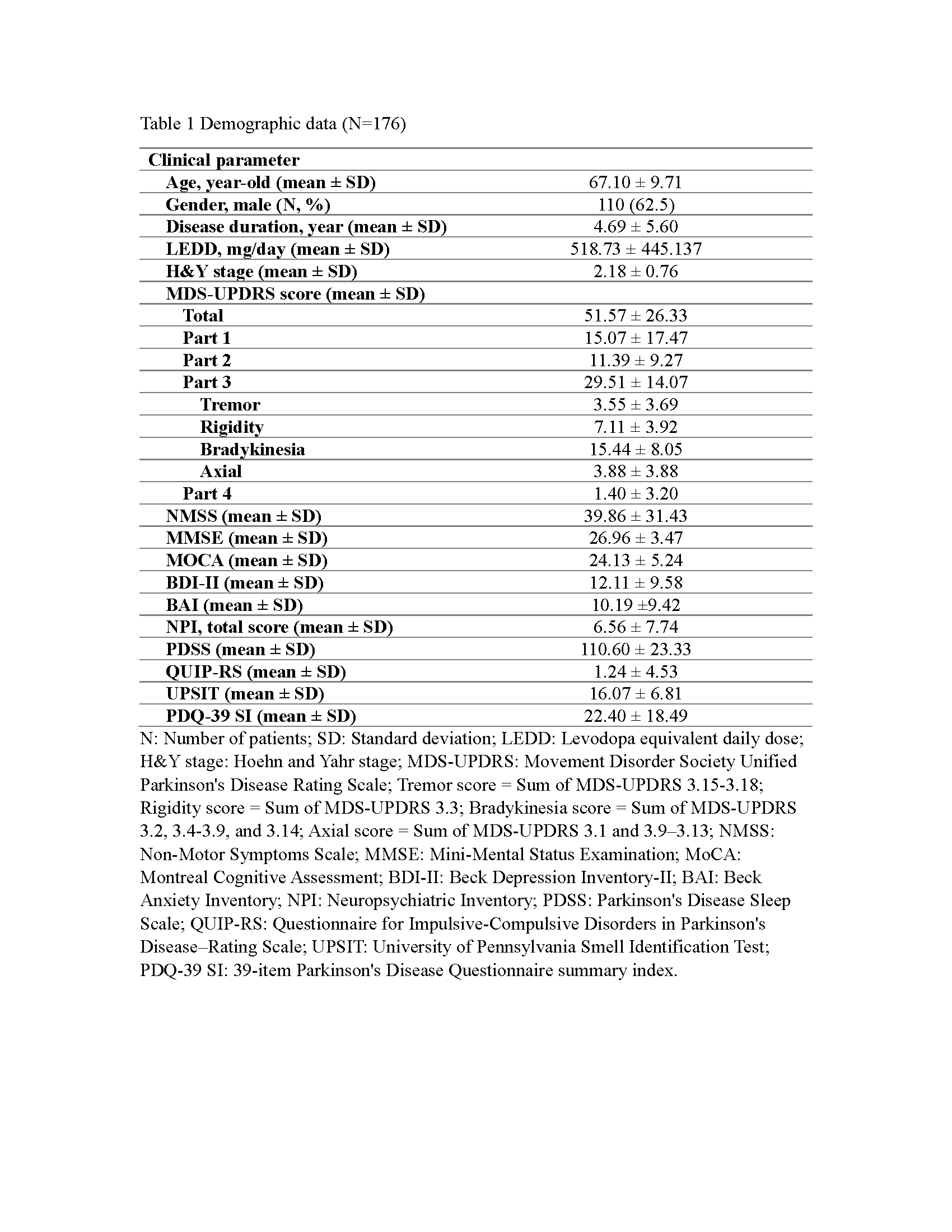
Results: A total of 176 PD patients were enrolled [Table 1]. The identification status of 18 odors in the UPSIT exhibited correlations with PD symptoms [Table 2]. Misidentification of rubber tire and bubble gum was associated with increased scores in both motor and non-motor symptoms, while difficulty identifying pizza and orange was linked to elevated global and motor severity in PD. Loss of identification in seven odors, including rubber tire, pizza, watermelon, jasmine, peanut, turpentine, and peach, heightened the risk of rigidity severity. The inability to recognize rubber tire, bubble gum, mint, and menthol odors in the UPSIT showed a negative correlation with MoCA scores. Additionally, negative correlations were observed between odor misidentification status and non-motor symptom scores, such as leather odor vs PDSS, root beer odor vs BDI, and fish/pine odor vs QUIP-RS.
Conclusion: In this study, correlations were identified between eighteen odors in the UPSIT and PD symptoms. A positive correlation was observed between odor misidentification status and motor symptoms. Interestingly, specific odor misidentification status was associated with decreased non-motor severities in PD, including cognition, sleep, depression, and impulsive-compulsive scores. These findings contradict previous reports [2], suggesting that the impact of identification status in different odors may have varying effects on PD non-motor symptoms.
Table 2
Table 1
References: [1] Masala C, Solla P, Liscia A, Defazio G, Saba L, Cannas A, et al. Correlation among olfactory function, motors’ symptoms, cognitive impairment, apathy, and fatigue in patients with Parkinson’s disease. J Neurol. 2018;265(8):1764-71.
[2] Roos, D.S., et al., Hyposmia as a marker of (non-)motor disease severity in Parkinson’s disease. J Neural Transm (Vienna), 2019. 126(11): p. 1471-1478.
To cite this abstract in AMA style:
YG. Guo, SC. Chiu. Odor-specific symptoms in Parkinson’s disease – UPSIT odor identification status versus clinical severity. [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/odor-specific-symptoms-in-parkinsons-disease-upsit-odor-identification-status-versus-clinical-severity/. Accessed December 27, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/odor-specific-symptoms-in-parkinsons-disease-upsit-odor-identification-status-versus-clinical-severity/