Category: Parkinson's Disease: Non-Motor Symptoms
Objective: We aimed to determine different subtypes of Parkinson’s disease (PD) patients using clinical data from the appearance chronology of their non-motor and motor symptoms in a longitudinal cohort.
Background: Although the clinical diagnosis of PD is mainly based on motor signs, it is well recognized that non-motor symptoms (NMS) can precede motor symptoms (MS) by several years. The NMS variability in PD patients also suggests a key role in pre-determining the disease progression with different types of trajectories. To investigate these trajectories, we used the NMS Questionnaire (NMSQuest) [1] data collected from patients included in a French multicentre longitudinal cohort.
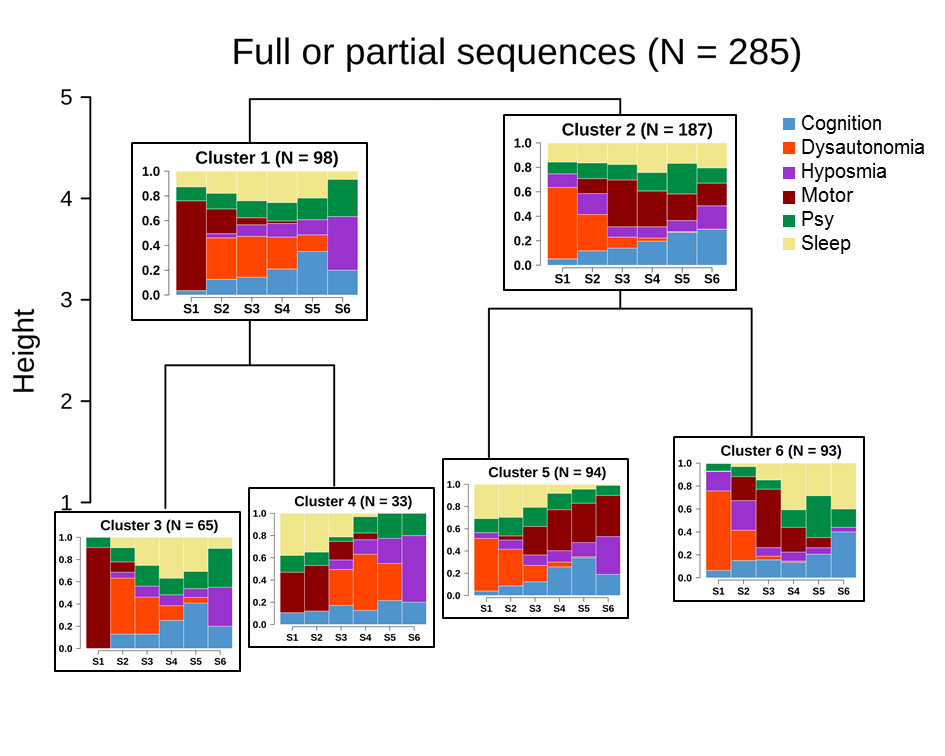
Method: DIGPD cohort [2] included 415 early PD patients with ≤5 years’ disease duration at baseline followed up annually up to 7 years. NSMQuest was addressed to patient at each visit. At baseline, patients were asked to provide the age at onset of each NMS if present before the visit. To build NMS sequences, 23 NMSQuest items were grouped into 5 NMS categories: dysautonomia, hyposmia, sleep, psychiatric and cognitive disorders. The dates of MS onset and initial NMS of each category were ranked from 1 to 6 to assign each subject an NMS sequence. Hierarchical clustering was then conducted on 285 subjects with at least 3 reported NMS categories using the Kendall’s Tau distance to measure rank agreement between all pairs of NMS sequences. At last, each derived cluster was characterized by its most representative NMS sequences and relevant clinical features.
Results: Cluster analysis of sequences revealed a clear separation between two main clusters, one ‘motor’ of 98 PD patients with earlier MS and one ‘dysautonomous’ of 187 PD patients with a NMS (mainly dysautonomia) before MS onset and a higher age at onset (60.7 ± 8.8 yo vs. motor: 56.2 ± 11.6 yo; p = 7.7e-4). Noteworthy, each cluster then subdivided into two subclusters based on sleep category. Of the two ‘dysautonomous’ subclusters, a group of 94 PD patients was found to be consistent with the Braak’s model [3,4]. [figure1]
Conclusion: NMS sequence clustering revealed two main profiles of ‘dysautonomous’ and ‘motor’ PD patients. Replication in other PD cohorts is an ongoing work to validate the clusters. Further cross-sectional analysis of the NMS clusters with biological data collected in DIGPD is also expected to identify new biomarkers and molecular signatures towards a better understanding of PD evolution.
References: [1] Martinez-Martin P, Schapira AHV, Stocchi F, et al. Prevalence of non-motor symptoms in Parkinson’s disease in an international setting; study using non-motor symptoms questionnaire in 545 patients. Mov Disord. 2007;22:1623–9. [2] Corvol J-C, Artaud F, Cormier-Dequaire F, et al. Longitudinal analysis of impulse control disorders in Parkinson disease. Neurology. 2018;91:e189–e201. [3] Braak H, Tredici KD, Rüb U, de Vos RAI, Jansen Steur ENH, Braak E. Staging of brain pathology related to sporadic Parkinson’s disease. Neurobiol Aging. 2003;24(2):197–211. [4] Braak H, Del Tredici K. Invited article: nervous system pathology in sporadic Parkinson disease. Neurology 2008;70:1916-1925.
To cite this abstract in AMA style:
H. You, F.X Lejeune, F. Danjou, S. Bekadar, J.C Corvol. Non-motor symptoms in Parkinson’s disease and the model of Braak [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/non-motor-symptoms-in-parkinsons-disease-and-the-model-of-braak/. Accessed January 5, 2026.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/non-motor-symptoms-in-parkinsons-disease-and-the-model-of-braak/