Session Information
Date: Monday, October 8, 2018
Session Title: Parkinson's Disease: Cognition
Session Time: 1:15pm-2:45pm
Location: Hall 3FG
Objective: To explore the role of clinical neuropsychological tools in Parkinson’s disease-dementia (PDD) vs. dementia with Lewy bodies (DLB). First, to define the feasibility of Mini-Mental State Examination (MMSE) and Montreal Cognitive Assessment (MoCA), which are the two most commonly used global cognitive scales. Second, to investigate which cognitive tests are the most sensitive in distinguishing PDD and DLB profiles.
Background: DLB represents the second most frequent neurodegenerative dementia among the elderly and shares with PDD common pathophysiologic substrates, resulting in the still open debate whether they are distinct diseases (Boeve et al., 2016).
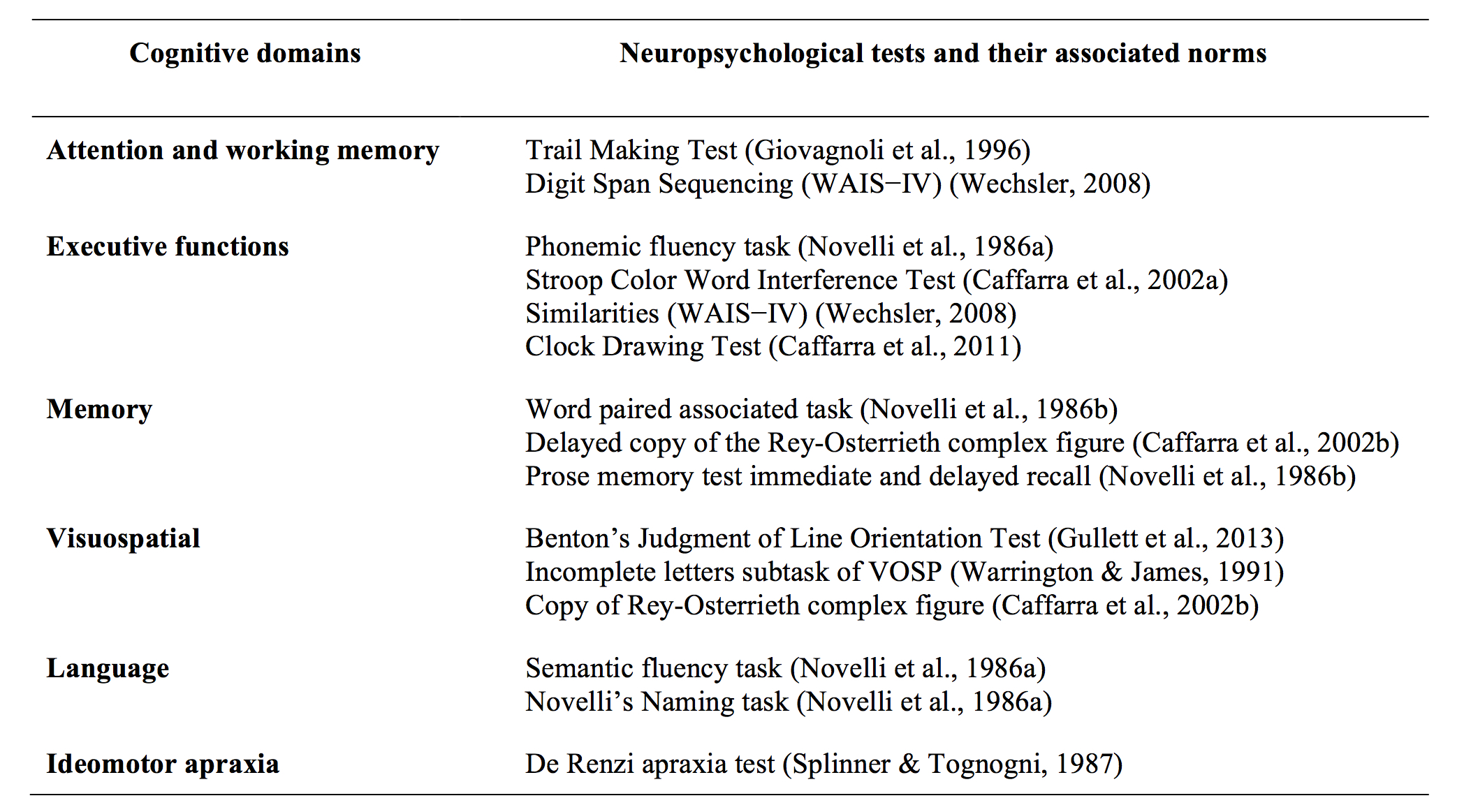
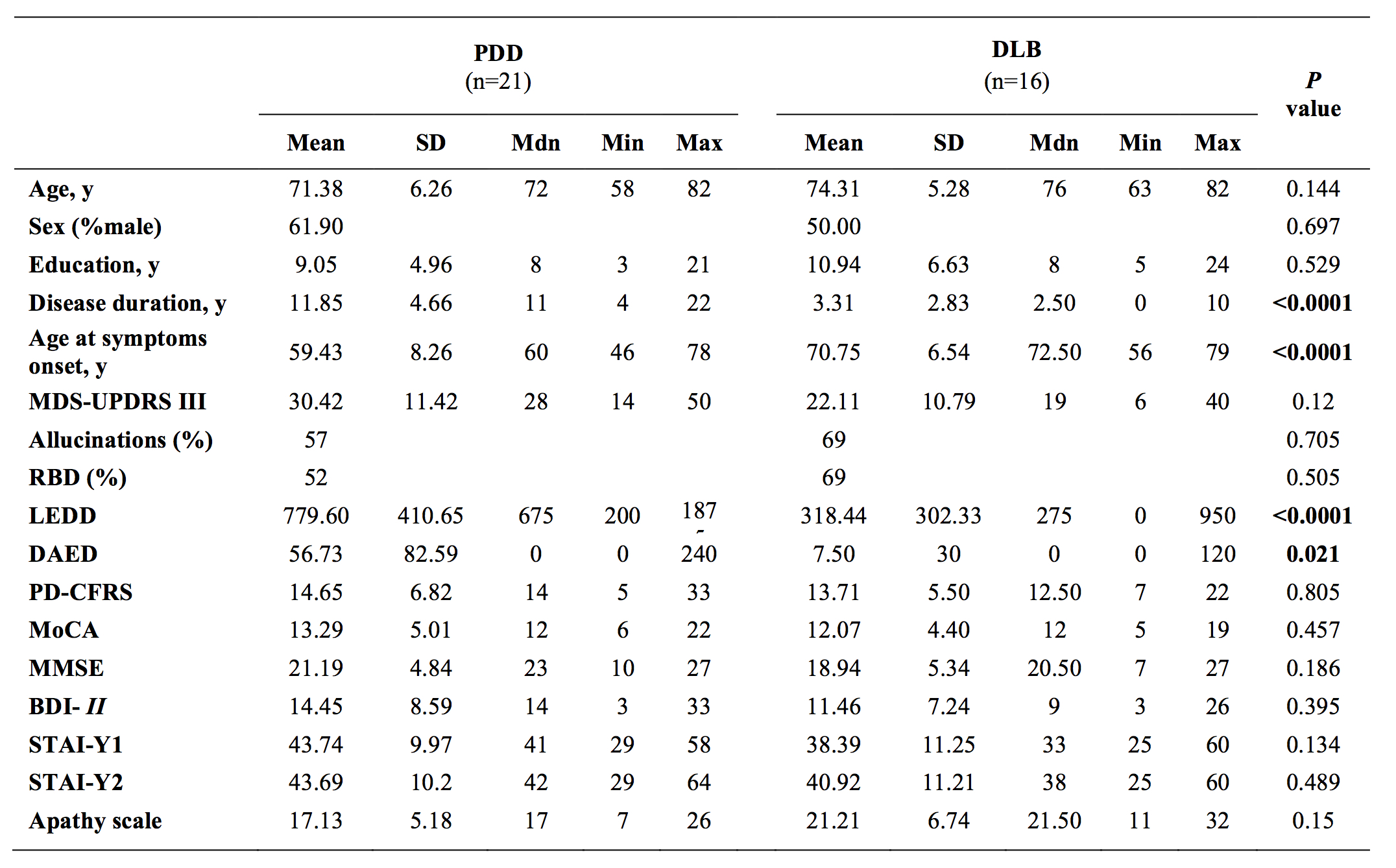
Methods: Twenty-one PDD patients referred consecutively, and 16 DLB matched for age, education and sex underwent clinical and neuropsychological assessment. An extensive neuropsychological battery, including MMSE and MoCA, was administered to assess cognitive deficits according to Level II criteria (Litvan et al., 2012) [table1].
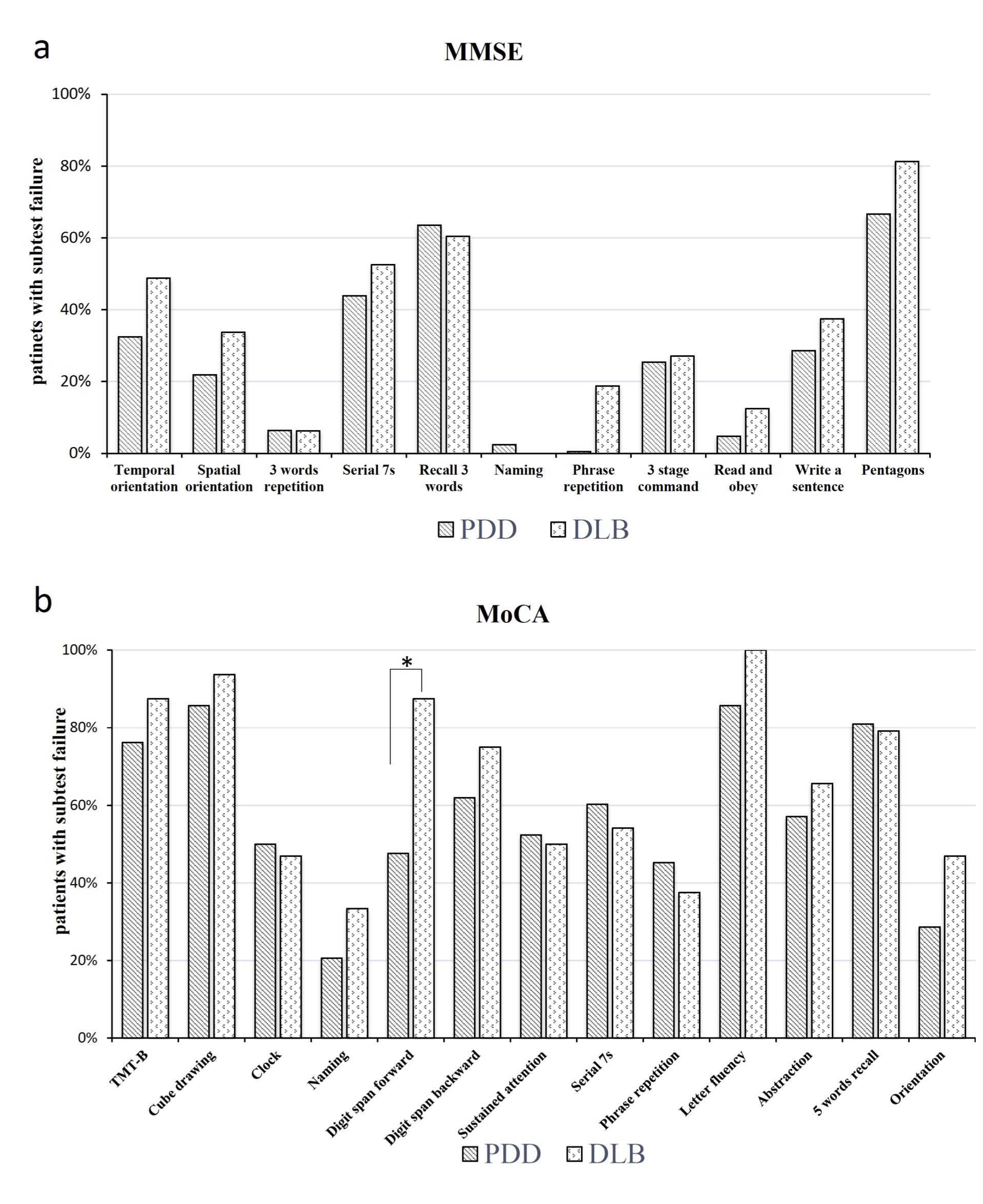
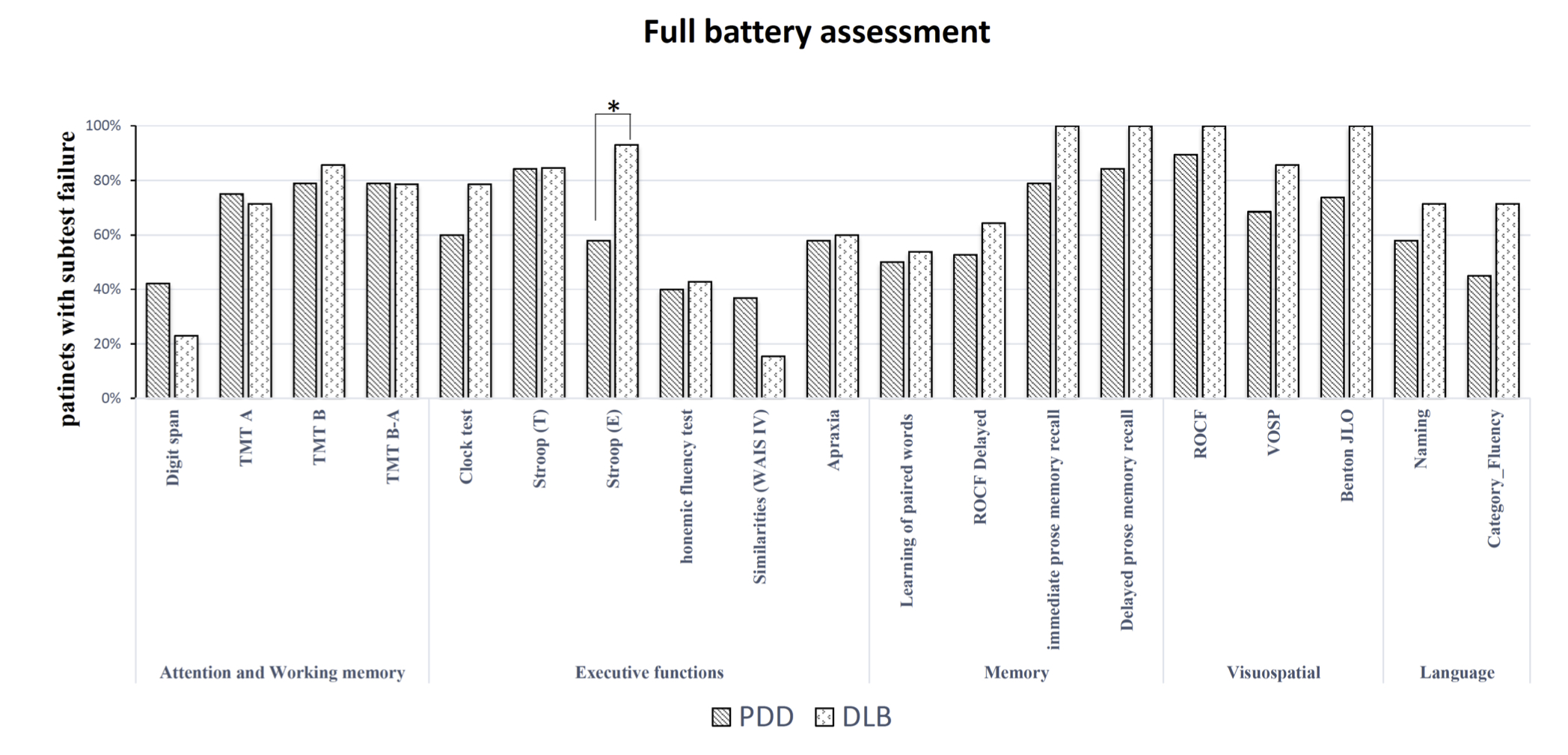
Results: Demographic and clinical characteristics are shown in [table2]. MoCA subitems’ analyses showed that DLB patients had worse performance in the Digit Span Forward subitem (p = 0.03), while there were no differences in the MMSE subitems [figure1]. Among all cognitive tests only the Stroop test (error) differentiated performance between PDD and DLB [figure2], wherein DLB patients made more errors than PD in execution time. Receiver-Operating Characteristic (ROC) analyses showed that the Stroop test (error) has a good sensitivity (0.92) but a lower specificity (0.51) in discriminating DLB from PDD, using a z-score cut-off equal to -2.66. Noteworthy, combining cognitive measures to clinical variables, the ROC analysis revealed a high specificity (0.90) and moderate sensitivity (0.75) in differentiating DLB from PDD patients. Disease duration (lower than 6-year), age at disease onset (> 67 years) together with Stroop test (error), are suggestive of DLB diagnosis.
Conclusions: MoCA is more sensitive than MMSE in detecting cognitive alterations in presence of frank dementia. Neuropsychological assessment (specifically Stroop test error) is a useful tool in the differential diagnosis between PDD and DLB.
References: Boeve, B. F., Dickson, D. W., Duda, J. E., Ferman, T. J., Galasko, D. R., Galvin, J. E., … & Kantarci, K. (2016). Arguing against the proposed definition changes of PD. Movement Disorders, 31(11), 1619-1622. Litvan, I., Goldman, J. G., Tröster, A. I., Schmand, B. A., Weintraub, D., Petersen, R. C., … & Aarsland, D. (2012). Diagnostic criteria for mild cognitive impairment in Parkinson’s disease: Movement Disorder Society Task Force guidelines. Movement disorders, 27(3), 349-356.
To cite this abstract in AMA style:
E. Fiorenzato, L. Weis, V. Camparini, F. Pistonesi, R. Schifano, E. Gasparoli, A. Antonini, R. Biundo. Neuropsychological and clinical assessment for the differential diagnosis of patients with PDD vs. DLB [abstract]. Mov Disord. 2018; 33 (suppl 2). https://www.mdsabstracts.org/abstract/neuropsychological-and-clinical-assessment-for-the-differential-diagnosis-of-patients-with-pdd-vs-dlb/. Accessed December 20, 2025.« Back to 2018 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/neuropsychological-and-clinical-assessment-for-the-differential-diagnosis-of-patients-with-pdd-vs-dlb/