Category: Parkinson's Disease: Neuroimaging
Objective: The aim of the study was to identify the mainly brain regions involved in postural instability (PI) in Progressive Supranuclear Palsy (PSP) with a Voxel Based Morphometry approach (VBM).
Background: PI is a core symptom in PSP [1] and it represents one of the most disabling symptoms in Parkinson’s Disease (PD) [2]. For this reason, PSP and PD, especially in their early stages, show overlapping clinical manifestations [3].
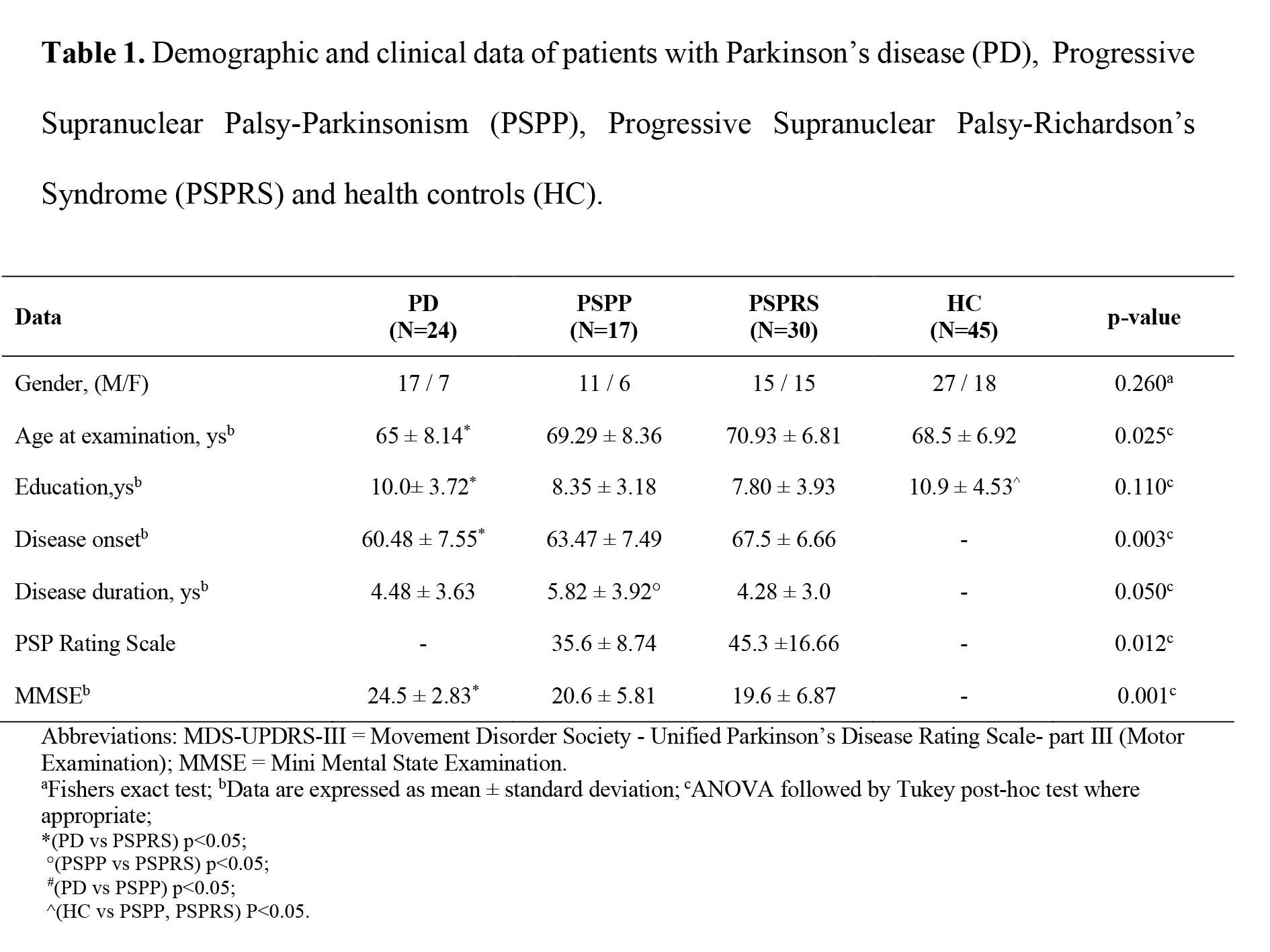
Method: We consecutively enrolled 47 PSP patients (30 PSP-Richardson’s syndrome [PSP-RS] and 17 PSP-Parkinsonism [PSP-P]), 24 PD patients without PI and 45 health controls. A whole-brain multi-regression VBM [4] analysis was used to identify brain areas where grey matter (GM) volume correlated with the postural stability (PS) score (item 27 of PSP-Rating Scale) in PSP patients. VBM, with a two-sample t-test, was also used to compare PSP-RS patients with PD patients. Finally, the associations between PS score and the GM volume in regions of interest (ROIs) extracted from the VBM contrast between PSP-RS and PD patients were investigated using linear correlation analysis.
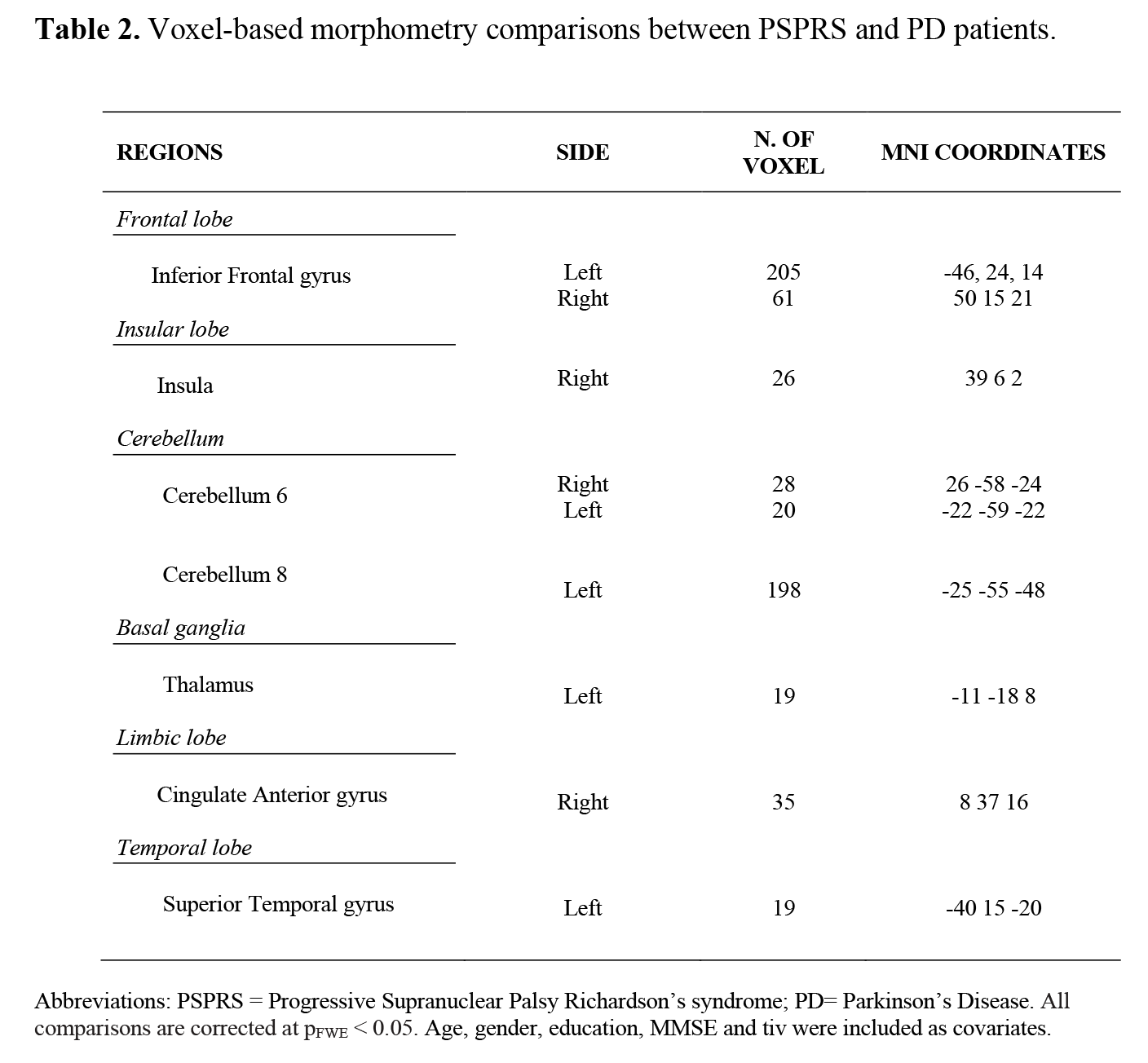
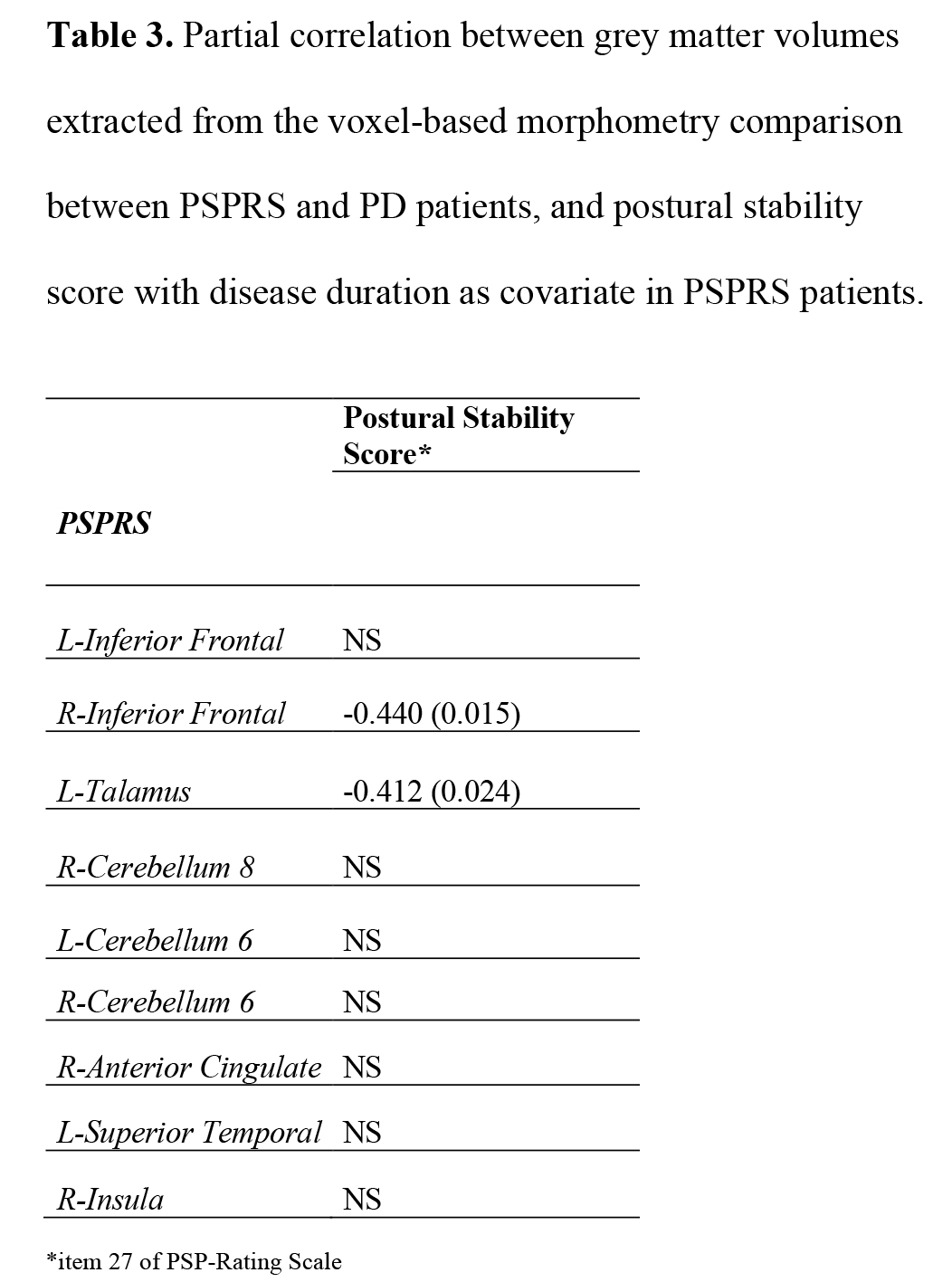
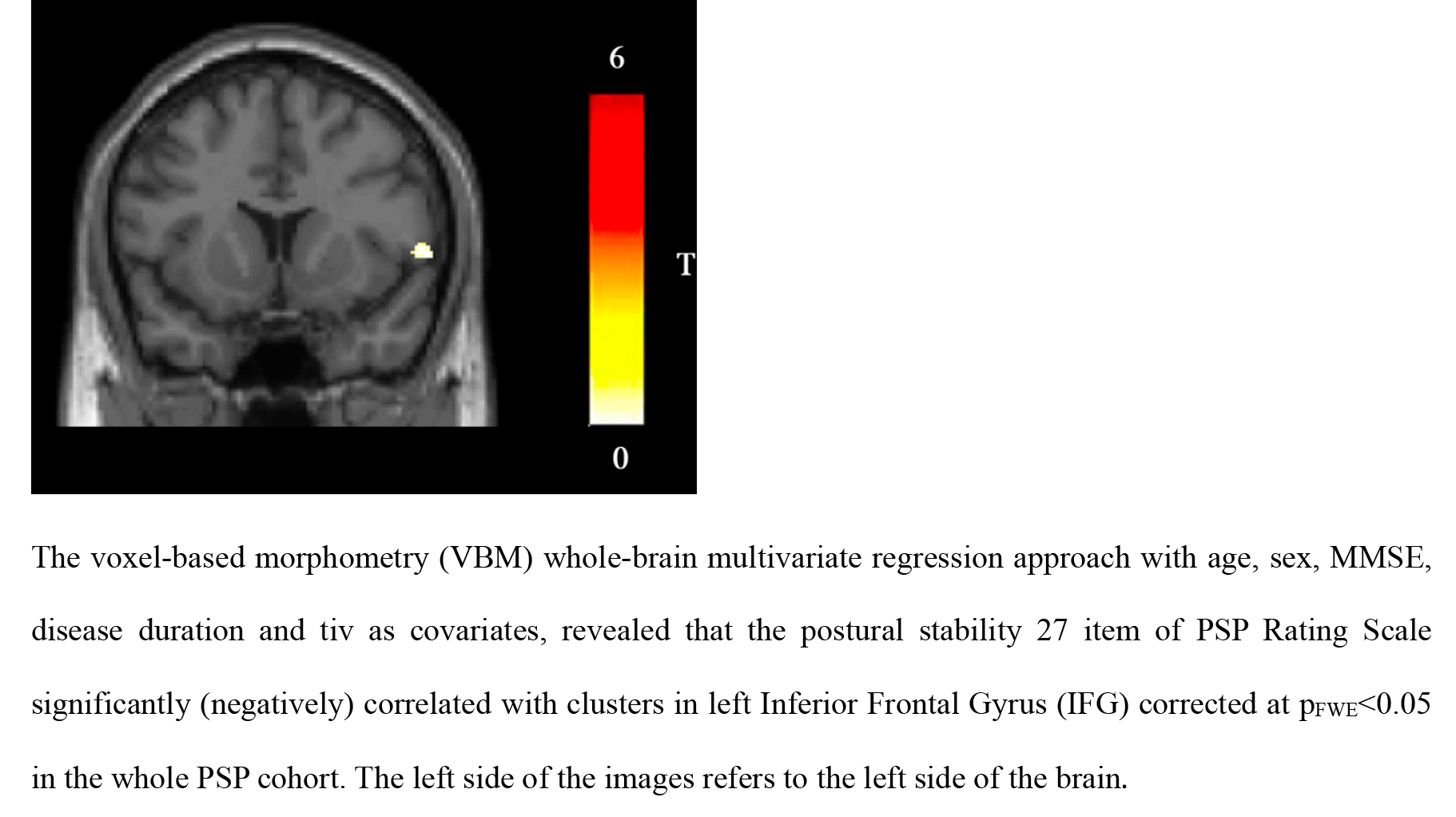
Results: Demographical data showed a significant difference in age and MMSE [Table 1]. VBM contrast between HC and PSP found various GM atrophy in PSP, while HC between PD were not different. Whole-brain multi-regression VBM analysis identified the inferior frontal gyrus (IFG) as the only region associated with PS score in PSP patients at pFWE<0.05 using age, gender, tiv, MMSE, disease duration as covariates [Figure 1]. The comparison between PSP-RS and PD patients showed reduced GM volume in fronto-temporal areas (including IFG), basal ganglia, limbic lobe, temporal lobe, and cerebellum at pFWE<0.05 using age, gender, education, tiv, MMSE as covariates [Table 2]. Among the ROIs extracted from the PSP-RS versus PD comparison, the IFG and thalamus were the only regions significantly (negatively) correlated with the PS score in PSP-RS patients using disease duration as covariate [Table 3].
Conclusion: This study provides neuroimaging evidence about the GM atrophy in PSP then PD patients in many regions and the involvement of the IFG and thalamus in the PI in PSP patients. This finding may be relevant to understand the pathophysiological mechanisms underlying postural instability and paves the way for ulterior studies on PI in parkinsonism.
References: [1] Höglinger GU, Respondek G, Stamelou M, et al. Clinical diagnosis of progressive supranuclear palsy: The movement disorder society criteria. Mov Disord. 2017; 32: 853-864. doi: 10.1002/mds.26987.
[2] Kim SD, Allen NE, Canning CG, et al. Postural instability in patients with Parkinson’s disease. Epidemiology, pathophysiology and management. CNS Drugs. 2013; 27: 97-112. doi: 10.1007/s40263-012-0012-3.
[3] Alster P, Madetko N, Koziorowski D, Friedman A. Progressive Supranuclear Palsy-Parkinsonism Predominant (PSP-P)-A Clinical Challenge at the Boundaries of PSP and Parkinson’s Disease (PD). Front Neurol. 2020 Mar 10;11:180. doi: 10.3389/fneur.2020.00180. PMID: 32218768; PMCID: PMC7078665.
[4] Dahnke R, Yotter RA, Gaser C. Cortical thickness and central surface estimation. Neuroimage. 2013 Jan 15;65:336-48. doi: 10.1016/j.neuroimage.2012.09.050. Epub 2012 Oct 3. PMID: 23041529.
To cite this abstract in AMA style:
C. Calomino, MG. Bianco, J. Buonocore, F. Aracri, M. de Maria, A. Sarica, A. Quattrone. Neuroimaging analysis of postural instability in Progressive Supranuclear Palsy: a Voxel‐based morphometry approach [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/neuroimaging-analysis-of-postural-instability-in-progressive-supranuclear-palsy-a-voxel%e2%80%90based-morphometry-approach/. Accessed January 17, 2026.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/neuroimaging-analysis-of-postural-instability-in-progressive-supranuclear-palsy-a-voxel%e2%80%90based-morphometry-approach/