Category: Rare Genetic and Metabolic Diseases
Objective: To correlate, clinical and magnetic resonance imaging (MRI) characteristics with genetics, of pediatric patients with Neurodegeneration with brain iron accumulation (NBIA).
Background: NBIA is a group of neurodegenerative disorders with excess iron in basal ganglia, substantia nigra (SN), red nucleus (RN) and dentate nucleus (DN), presents with clinical and genetic heterogenicity.
Method: 12 pediatric patients, with extrapyramidal features, spasticity, seizures and neuropsychiatric abnormalities in varying combinations with MRI evidence of iron deposition were included. Investigations such as serum ceruloplasmin, ferritin, hormonal profile, smear for acanthocytes, fundus/slit lamp examination, neuropsychological assessment, electroencephalogram and nerve conduction study were done according to the clinical presentation. Targeted/clinical exome gene sequencing was done.
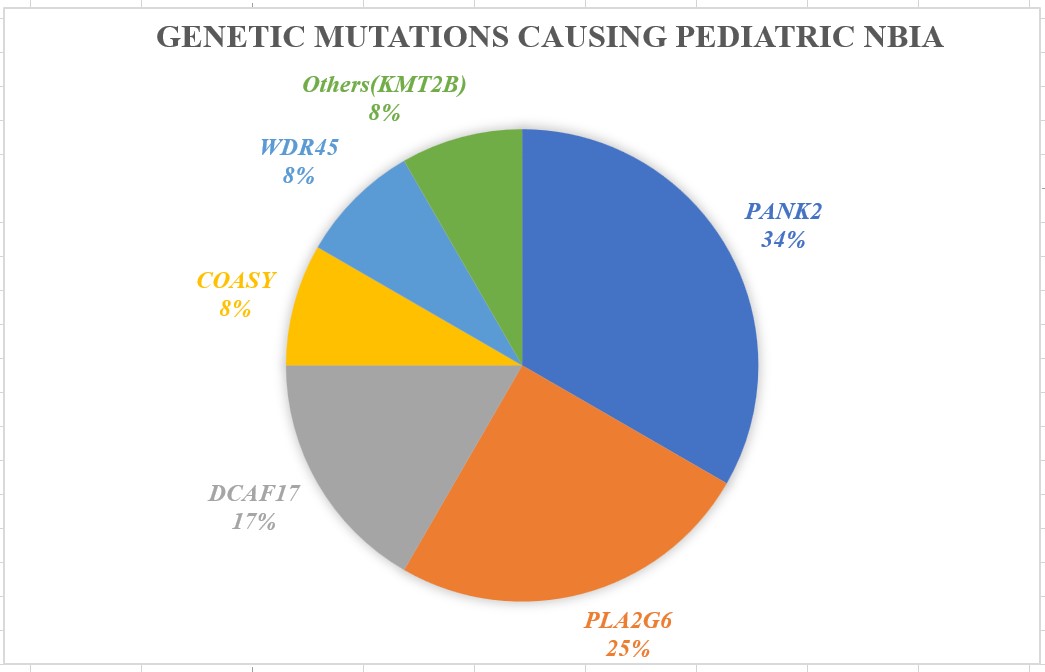
Results: 7/12 patients were males ,age of onset ranging from 2-12 years (7.94±3.62). 7 were consanguineous born and 3 had a positive family history. First symptom was dystonia in 11 (all limb onset), and spastic-ataxia in 1. Over the course of illness all had dystonia, 3 had parkinsonism, 2 had ataxia and 1 had hand stereotypies. Oculomotor abnormalities (the most common associated feature) included slow saccades (6) and oculomotor apraxia (1). Neuropsychiatric symptoms (4), pyramidal signs (3), optic disc pallor (1), seizures (1) and retinal pigmentary degeneration (1) were observed. Susceptibility weighted images (SWI) showed mineralisation of globus pallidus in all, substantia nigra in 9, combined RN, DN and striatum in 3. Three had classical “eye of the tiger” sign, 2 had bilateral white matter hyperintensities. Mutations were seen in PANK2 (4), PLA2G6 (3), DCAF17 (2), COASY (1), WDR45 (1) and 1 showed mutation in KMT2B.
Conclusion: Neuroimaging and ophthalmological evaluation provide important clues to NBIA diagnosis. PANK2-associated neurodegeneration(PKAN) was the commonest NBIA in pediatric population followed by PLA2G6-associated neurodegeration (PLAN).
Genetic mutations found in Pediatric NBIA
References: 1.Kurian MA, McNeill A, Lin JP, Maher ER. Childhood disorders of neurodegeneration with brain iron accumulation (NBIA). Dev Med Child Neurol. 2011 May;53(5):394-404.
To cite this abstract in AMA style:
D. Kalikavil Puthanveedu, A. Cherian. Neurodegeneration with brain iron accumulation in pediatric population: Clinico-radiologic and genetic features [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/neurodegeneration-with-brain-iron-accumulation-in-pediatric-population-clinico-radiologic-and-genetic-features/. Accessed April 20, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/neurodegeneration-with-brain-iron-accumulation-in-pediatric-population-clinico-radiologic-and-genetic-features/