Session Information
Date: Thursday, June 8, 2017
Session Title: Parkinson's Disease: Neuroimaging And Neurophysiology
Session Time: 1:15pm-2:45pm
Location: Exhibit Hall C
Objective: To explore the neural correlates sub-serving isolated minor hallucinations in Parkinson’s disease (PD) through a multimodal structural and functional neuroimaging approach based on grey matter volume (GMV) voxel-based morphometry (VBM) and resting-state fMRI (rs-fMRI).
Background: Minor hallucinations are a frequent symptom in PD. They occur in up to 50% of patients and can evolve into well-structured hallucinations as disease progresses [1]. Isolated minor hallucinations in PD have been associated with structural changes in the dorsal visual pathway in a single study using voxel-based morphometry [2]. However the neuroanatomical substrate of minor hallucinations remains poorly understood.
Methods: We studied a sample of 14 non-demented PD patients, with (PDmH, n = 7) and without (n = 7) minor hallucinations, matched by age, education, medication and cognition. Participants underwent (i) clinical and neuropsychological assessment; (ii) MRI scan using whole-brain VBM; and (iii) rs-fMRI seed-to-whole brain techniques. We compared GMV and functional connectivity relative to precuneus in both groups. Significance was set at p<0.005; k=50.
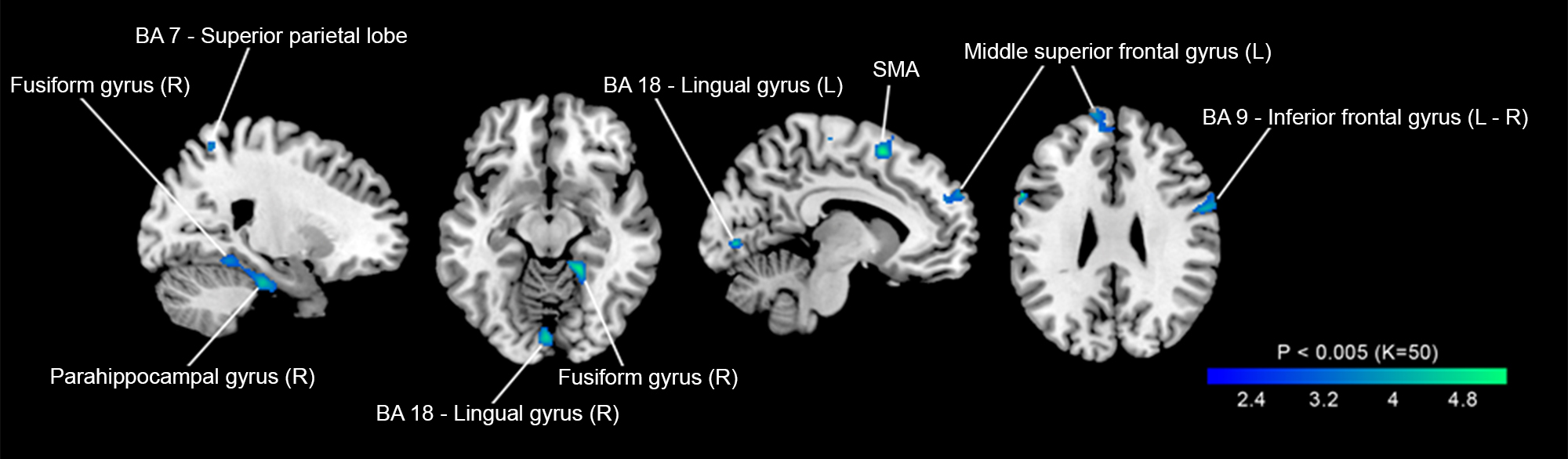
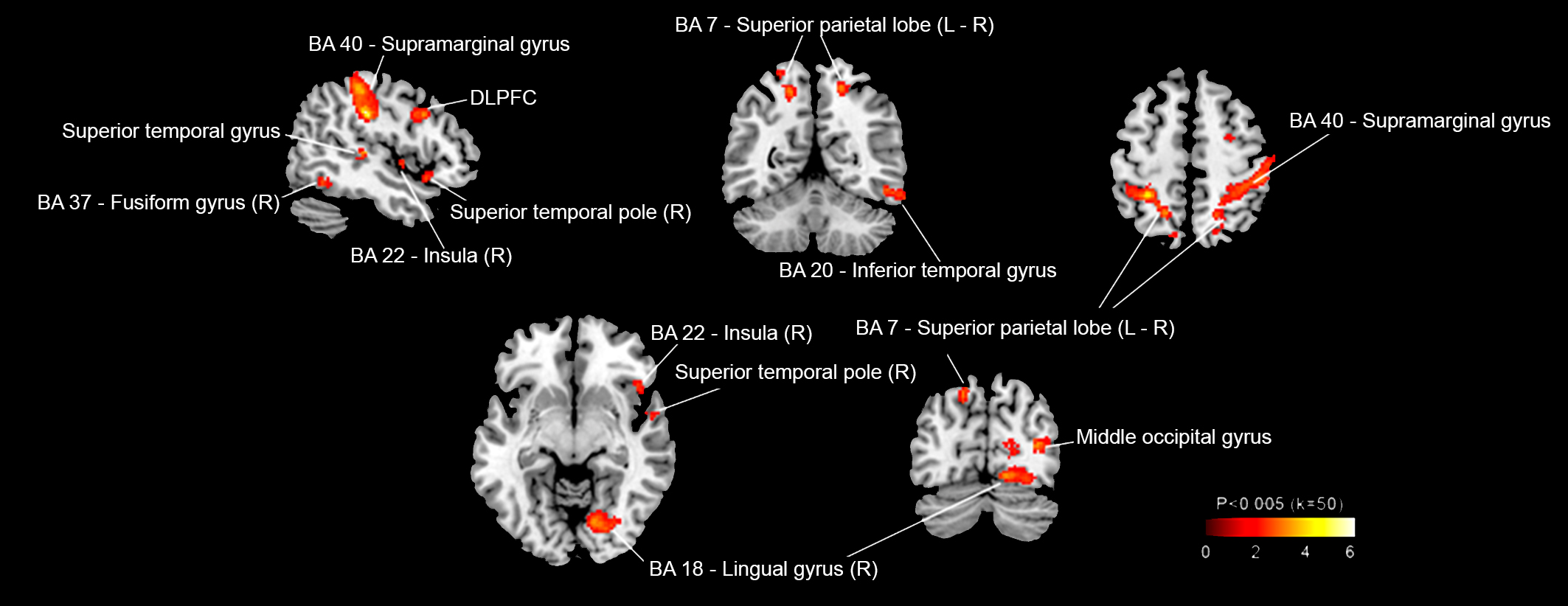
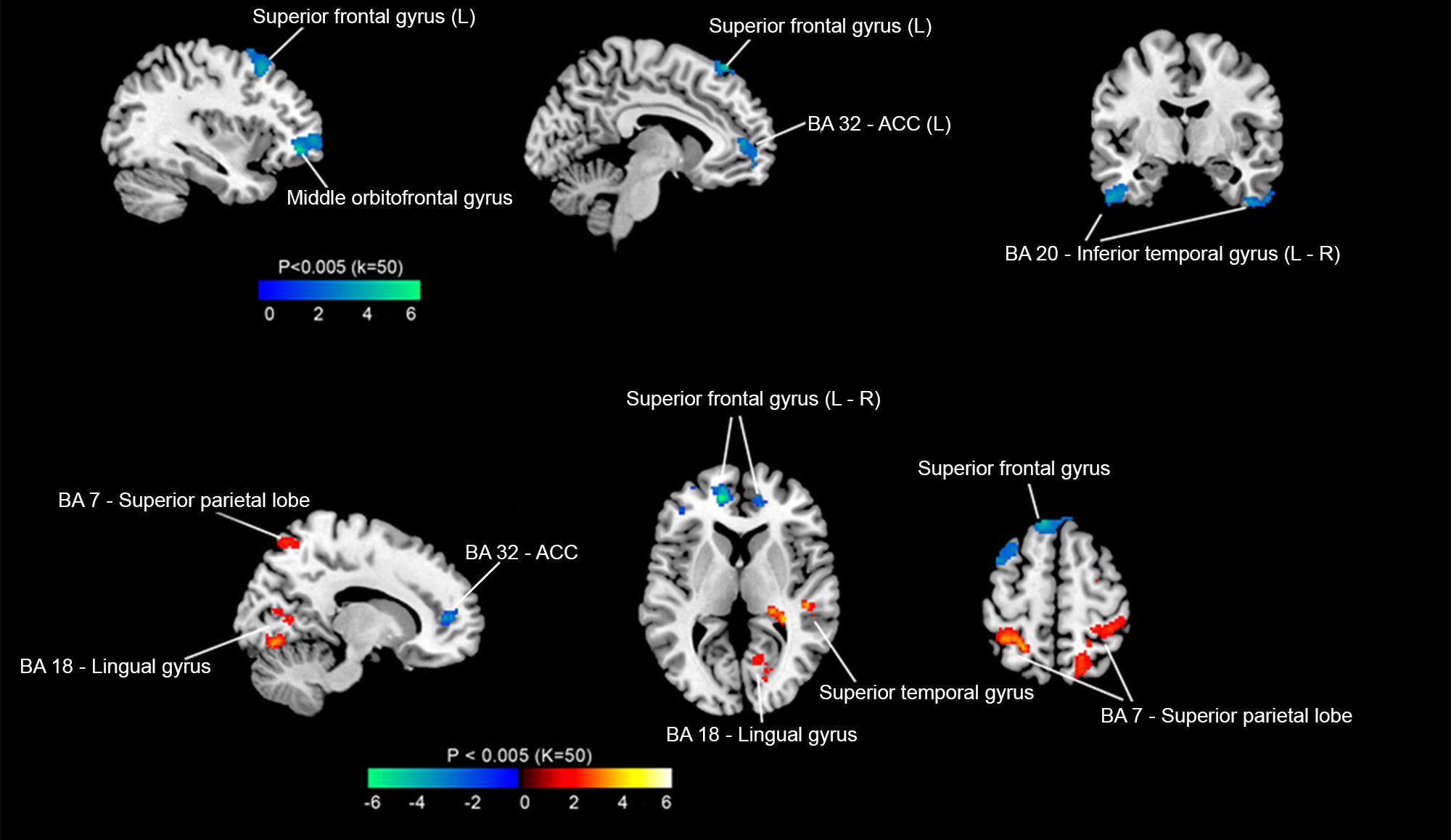
Results: Minor hallucinations were associated with GMV loss in dorsal and ventral visual pathways and in frontal areas [figure 1]. In the PDmH group, increased functional connectivity was found between precuneus and (i) dorsal and ventral visual pathways (superior parietal lobe, fusiform, lingual and inferior temporal gyrus); (ii) sensory processing transmodal areas (supramarginal gyrus, insula, superior temporal pole); and (iii) dorsal attention network (dorsolateral prefrontal cortex, intraparietal sulcus) [figure 2]. Conversely, decreased functional connectivity was found between precuneus and ventral attention network (anterior cingulate cortex, superior frontal gyrus) [figure 3].
Conclusions: Minor hallucinations are associated with structural and functional changes in sensory processing areas and attention networks. In addition to volume loss in both visual pathways, PDmH showed an increased functional connectivity between precuneus and posterior cortical regions (visuoperceptive integration areas and dorsal attention network) and decreased functional connectivity between precuneus and distant brain regions of ventral attention network.
References: [1] Christopher G. Goetz; Wenqing Fan; Sue Leurgans; Bryan Bernard; Glenn T. Stebbins. The Malignant Course of “Benign Hallucinations” in Parkinson Disease. Arch Neurol. 2006;63:713-716.
[2] Pagonabarraga J; Soriano-Mas C; Llebaria G; López-Solà M; Pujol J; Kulisevsky J. Neural Correlates Of Minor Hallucinations In Non-Demented Patients With Parkinson’s Disease. Parkinsonism and Related Disorders (2014), doi: 10.1016/j.parkreldis.2013.11.017.
To cite this abstract in AMA style:
H. Bejr-kasem, J. Pagonabarraga, S. Martinez-Horta, F. Sampedro, J. Marin-Lahoz, J. Perez-Perez, A. Horta-Barba, B. Pascual-Sedano, J. Kulisevsky. Neural correlates of minor hallucinations in Parkinson’s disease: A multimodal imaging study [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/neural-correlates-of-minor-hallucinations-in-parkinsons-disease-a-multimodal-imaging-study/. Accessed December 14, 2025.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/neural-correlates-of-minor-hallucinations-in-parkinsons-disease-a-multimodal-imaging-study/