Category: Myoclonus
Objective: To assess myoclonus phenomenology and its response to antiepileptic drugs in patients with SSPE.
Background: Myoclonus is one of the characteristic features of Sub Sclerosing Pan Encephalitis.1 Periodic and slow myoclonus is the pathognomic of SSPE.2 Myoclonic jerks are frequently associated with falls and interfere with daily life activities, even in the early stages of SSPE. Myoclonus in some patients is refractory to treatment, and we still lack evidence-based recommendations for using antiepileptics in SSPE. Although carbamazepine is known to exacerbate myoclonus, it is often effective in SSPE with refractory myoclonus.3, 4 We aimed to look into the myoclonus phenomenology, its response to AED, and its predictors.
Method: We conducted the prospective study from Sep 2021 to Dec 2022 at a tertiary care center in India. The institutional ethics committee approved the study. We enrolled 45 patients with SSPE. Patients were diagnosed based on Dyken’s Criteria and staged as per Jabbour’s staging system. Patients were given valproate, levetiracetam, and clonazepam alone or in various combinations. Patients were also given intrathecal interferon-alpha. We analyzed the myoclonus phenomenology as per the historical and video graphic details.
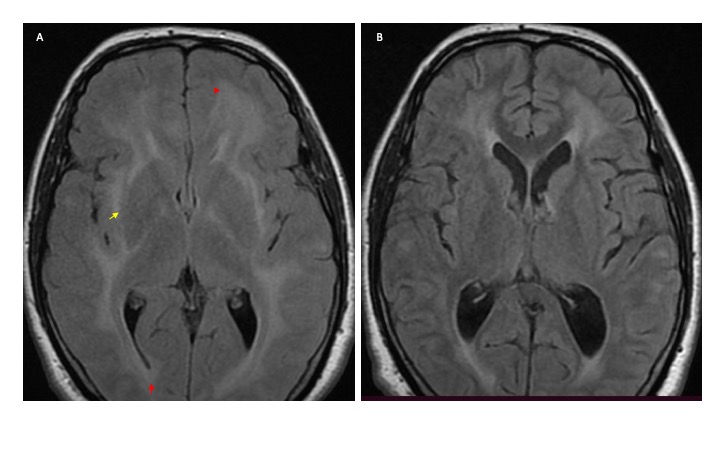
Results: The mean age of the study population was 14.44±6.81 years. Eighty percent were males. Thirty-four patients (75.6%) were in Jobbour’s stage-3. Myoclonus was present in 42 (93.33%) patients. Generalized myoclonus was the commonest 18 (~43%), followed by segmental and truncal myoclonus in 6 (14.2%) and 5(~12%) patients. Hemi myoclonus, jaw opening, and neck myoclonus were observed in 12 patients (4 in each group). Generalized seizures were seen in 16 (35.6%). Subcortical white matter hyperintensities were the most typical neuroimaging finding in 33 (73.33%) patients (Figure). Sodium valproate was the commonest drug used in 40 (~89%) patients, followed by clonazepam and levetiracetam. Carbamazepine was used in six patients. Reduction in myoclonus was observed in 27 (~64%) patients, whereas 15 (~36%) had no response. Three of six patients on carbamazepine responded.
Conclusion: Refractory myoclonus is observed in a significant number of patients with SSPE. Generalized myoclonus with the fulminant course and slow EEG background are frequently refractory. Seizures are rare. Evidence-based antiepileptic drug recommendations are warranted in SSPE.
References: 1. Vela L, Garcia-Merino A, Escamilla C. Adult-onset subacute sclerosing panencephalitis first seen as craniocervical myoclonus. Movement disorders: official journal of the Movement Disorder Society. 1997 May;12(3):462-4.
2. Gupta D, Gupta H, Patel A, Dugani P, Pradeep R, Mehta A, Javali M, Acharya PT, Srinivasa R. Teaching Video NeuroImage: Slow Axial Myoclonus in Subacute Sclerosing Panencephalitis. Neurology. 2022 Nov 8;99(19):864-5.
3. Schimmel M, Penzien J. Improvement of SSPE after carbamazepine: natural course or therapeutic effect?. Neuropediatrics. 2010 Aug;41(02):P1380.
4. Ravikumar S, Crawford JR. Role of carbamazepine in the symptomatic treatment of subacute sclerosing panencephalitis: a case report and review of the literature. Case Reports in Neurological Medicine. 2013 Mar 7;2013.
To cite this abstract in AMA style:
S. Pandey, K. Db, R. Garg, H. Malhotra, A. Jain, S. Kumar. Myoclonus Phenomenology and its Response to Antiepileptic drugs in Patients with Sub acute Sclerosing Pan encephalitis [abstract]. Mov Disord. 2023; 38 (suppl 1). https://www.mdsabstracts.org/abstract/myoclonus-phenomenology-and-its-response-to-antiepileptic-drugs-in-patients-with-sub-acute-sclerosing-pan-encephalitis/. Accessed December 28, 2025.« Back to 2023 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/myoclonus-phenomenology-and-its-response-to-antiepileptic-drugs-in-patients-with-sub-acute-sclerosing-pan-encephalitis/