Objective: To compare subgroups of patients with Parkinson’s disease (PD) with and without rapid eye movement sleep behavior disorders (RBD), in terms of progression speed, age at onset and ordering of abnormalities.
Background: Subtypes of patients with PD, e.g. with and without RBD have different patterns of progression. A better characterization of these patterns may have important prognostic implication.
Method: We selected 349 consecutive idiopathic PD patients from the PPMI Dataset (www.ppmi-info.org/data). Patients that reached a REM-quizz score of 6 over 9 at least once over the course of the study were labeled as RBD+ (94 patients), the others as RBD- (249 patients). These two groups were compared based on the MDS-UPDRS part III, MoCA, SCOPA-AUT, REM-quizz and the Striatal Binding Ratios (SBR) of left and right side of both Putamen and Caudate.
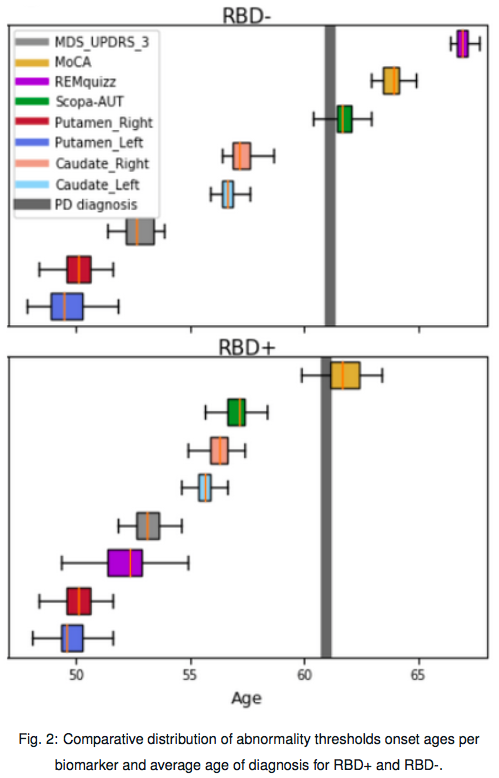
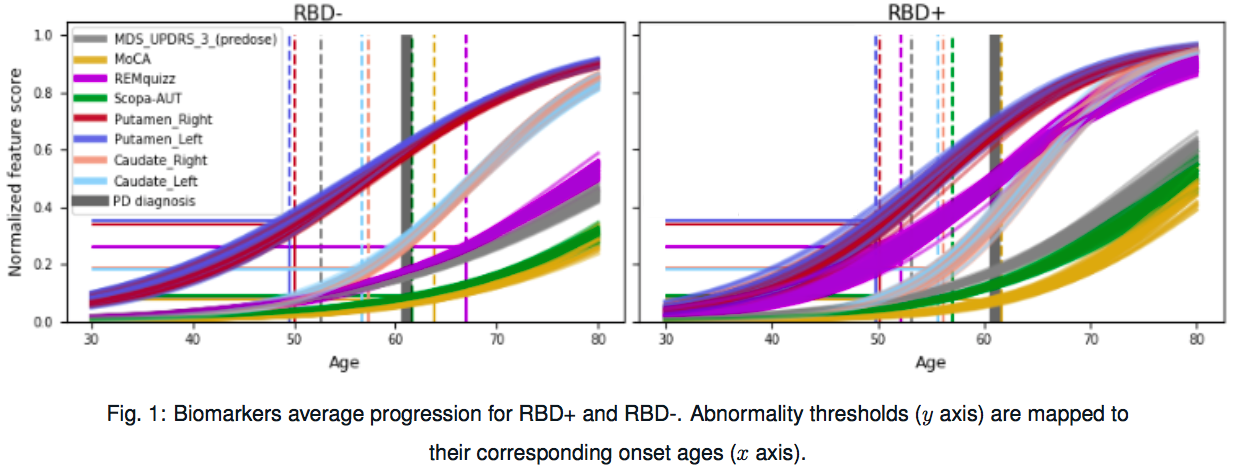
A statistical Bayesian model was used to estimate the longitudinal average progression of clinical and imaging scores for both groups. For each biomarker, abnormality thresholds were computed from the data as the optimal cut-off between PD patients and controls at baseline. Then, these thresholds were mapped to their corresponding average age of abnormality occurrence within each group using the respective group-average trajectories.
[figure1]
A resampling procedure (10×5 cv) allows to get confidence interval on the arrival of abnormalities of PD biomarkers for both groups.
[figure2]
Results: First, from the estimated individual parameters we found that RBD+ were affected in average 6 years earlier than RBD-, and progressed 30% faster. Yet RBD+ were diagnosed in average at the same age, meaning that at time of diagnosis RBD+ were more advanced than RBD-, which is confirmed by comparing subgroups at baseline. Second, the ordering of abnormalities between modalities in the two groups was the same, REM-quizz excepted. The abnormalities were observed first in the putamen, then in MDS-UPDRS part III, caudate, scopa and finally MoCA. Abnormalities in the MoCA and SCOPA-AUT occurred up to four years earlier for RBD+. At the same stage of the disease, RBD+ patients were more affected for the REM and Scopa-aut scales, whereas RBD- patients were more affected for the MDS, MoCA and DAT scales.
Conclusion: PD patients with RBD progressed faster and started disease earlier than PD without RBD. They also showed a different pattern of progression of the disease.
References: R. B. Postuma, A. E. Lang, J. F. Gagnon, A. Pelletier, J. Y. Montplaisir. How does parkinsonism start? Prodromal parkinsonism motor changes in idiopathic REM sleep behaviour disorder. Brain, Volume 135, Issue 6, June 2012, Pages 1860–1870 J.-B. Schiratti, S. Allassonnière, O. Colliot, S. Durrleman. A Bayesian mixed-effects model to learn trajectories of changes from repeated manifold-valued observations. Journal of Machine Learning Research, 18(133):1-33. 2017. R. Couronné, M. Vidailhet, J.C. Corvol, S. Lehéricy, S. Durrleman. Learning disease progression models with longitudinal data and missing values. ISBI. 1033-1037. 2019. Marek, K., Jennings, D., Lasch, S., Siderowf, A., Tanner, C., Simuni, T., … & Poewe, W. (2011). The parkinson progression marker initiative (PPMI). Progress in neurobiology, 95(4), 629-635.
To cite this abstract in AMA style:
R. Couronné, A. Valladier, M. Vidailhet, J.C Corvol, S. Lehericy, S. Durrleman. Multimodal model of Parkinson’s disease highlights differences in progression profiles of RBD patients [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/multimodal-model-of-parkinsons-disease-highlights-differences-in-progression-profiles-of-rbd-patients/. Accessed March 6, 2026.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/multimodal-model-of-parkinsons-disease-highlights-differences-in-progression-profiles-of-rbd-patients/