Session Information
Date: Tuesday, June 6, 2017
Session Title: Therapy in Movement Disorders
Session Time: 1:45pm-3:15pm
Location: Exhibit Hall C
Objective: The purpose of this program was to analyze whether activities of daily living (ADL) could be improved, thereby delaying definite nursing home admission and reducing costs.
Background: Parkinson’s disease (PD) is a progressive neurodegenerative disorder. PD patients typically develop serious physical and neuropsychiatric impairments and eventually lose their ability to live independently. To take care of advanced PD patients with multiple problems that negatively interfere with independent living, a multidisciplinary program, including a ‘customized’ program and optimization of medication, was started at the Rehabilitation Unit of the Parkinson Expertise Center (RU-PEC) in Groningen.
Methods: A total of 24 advanced PD patients (13 men and 11 women), median age of 71 years (range 57-84 years) were included in this program. Assessments were performed at baseline and 6 weeks, 3 months, 2 and 5 years after inclusion. Primary endpoints of the study were improvement of the ADL, measured with the AMC Linear Disability Scale (ALDS) and ability of the patients to live independently at home after participation in the RU-PEC program. Secondary endpoints included the cost-effectiveness of this program, as measured by a cost assessment battery.
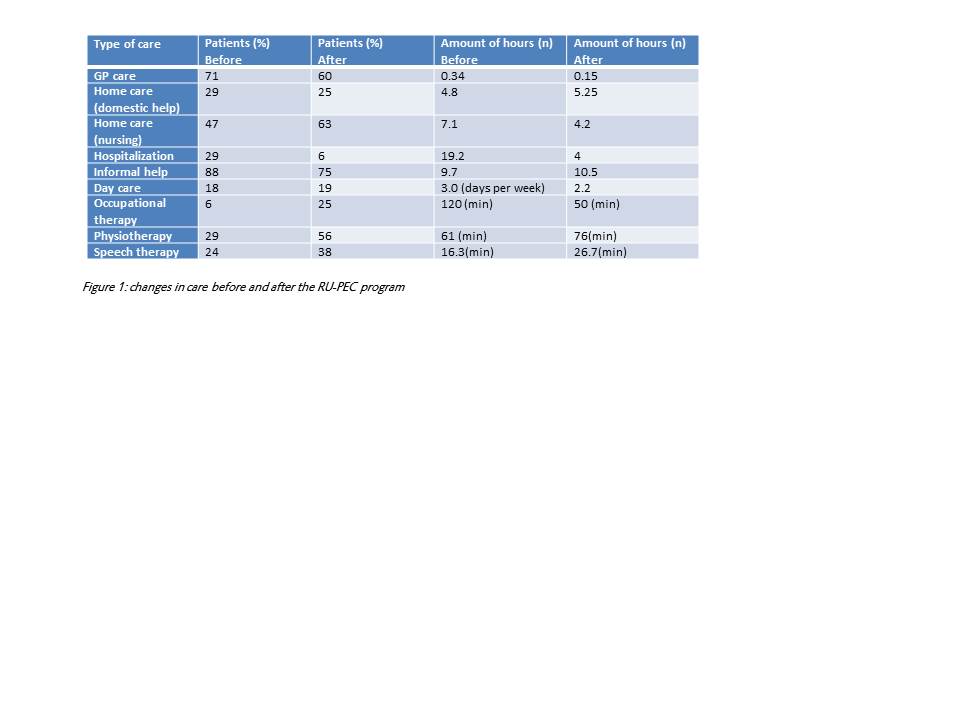
Results: A total of 83% of the patients could return home after participation in the RU-PEC program. After 2 years, 65%, and 5 years after completion of the RU-PEC program 28% of the patients were still able to live independently at home. The ALDS score improved with a mean of 9.9 points (Cl 95%, P=.0001). This improvement was observed in 78% of the included patients. Figure 1 shows the reductions and increases of therapies and needed care at home after dismission from the RU-PEC. Annual costs of Parkinson care in 2011 in the Netherlands were estimated at 267 million euro (RIVM, 2013). 70% of these costs go to elderly care (nursing home) and 11% of these costs are spent on care at home. If elderly PD patients could live longer independently at home, costs of Parkinson care would reduce enormously. Overall these changes lead to a better quality of life and a reduction of overall costs.
Conclusions: The RU-PEC program effectively delayed nursing home admission of PD patients. Irrespective of the small increase of costs of care at home, the overall effect was a cost reduction per patient, which was primarily caused by the postponement of definite nursing home admission.
To cite this abstract in AMA style:
E. Steendam-Oldekamp, W. Rutgers, T. van Laar. Multidisciplinary Parkinson rehabilitation delays nursing home admission and is cost-effective. [abstract]. Mov Disord. 2017; 32 (suppl 2). https://www.mdsabstracts.org/abstract/multidisciplinary-parkinson-rehabilitation-delays-nursing-home-admission-and-is-cost-effective/. Accessed January 4, 2026.« Back to 2017 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/multidisciplinary-parkinson-rehabilitation-delays-nursing-home-admission-and-is-cost-effective/