Category: Parkinson's Disease: Neuroimaging
Objective: To assess the galvanic vestibular stimulation (GVS) effect on axial symptoms and cervical vestibular evoked myogenic potential (cVEMP) depending on the Magnetic Resonance Parkinsonism Index (MRPI) and Midbrain-Pons Ratio (MPR).
Background: . Axial symptoms in Parkinson’s disease (PD) such as freezing of gait (FOG), trunk rigidity and postural instability (PI) are often resistant to treatment. Due to the PD-related vestibular system abnormalities participate in PI and gait disorders, GVS could become an effective noninvasive treatment for these symptoms. However, some studies have shown that GVS does not always improve motor function in PD effectively. We hypothesized that the effectiveness of GVS may depend on the neurodegeneration severity, including in brainstem motor centers, and MRPI and MPR may provide valuable information about PD-related changes in the brain.
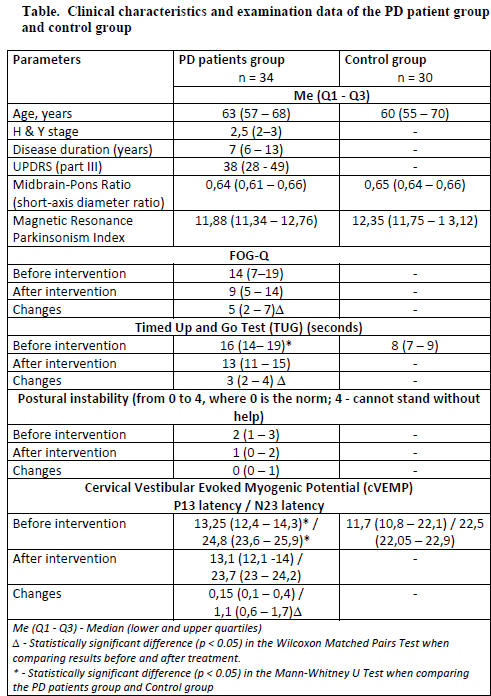
Method: Participants included 34 PD patients and 30 age-matched controls. Additionally to MRI-based measurements, we assessed the cVEMP parameters, FOG-Q, TUG test score and evaluated the PI severity in PD patients before and after a 12-session GVS course.
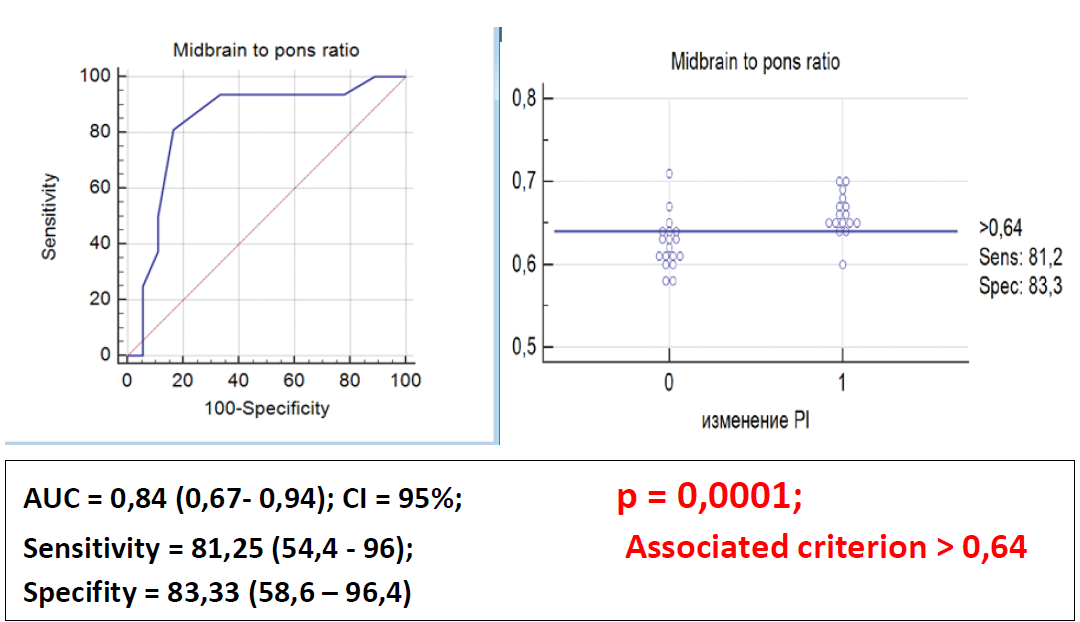
Results: PD patients had a significant delay in the cVEMP components latency compared to controls, indicating a slowdown in vestibulospinal conduction. Nevertheless, there were no differences between groups in MRPI and MPR (table). After the GVS course, an improvement was observed in FOG-Q and TUG test as well as a significant decrease in the N23 latency of the cVEMP in PD patients. These changes were independent of MRI data, whereas improvement in PI was dependent on MPR, and GVS was effective in PD patients with MPR > 0,64 (figure).
Conclusion: GVS, acting on vestibular afferent flows, improves vestibulospinal conduction and modifies the conflict between sensory systems, which ultimately has a positive effect on the severity of gait disorders. Therefore, GVS may become a clinically applicable non-invasive neuro-modulatory treatment for axial symptoms in PD. However, the ability of GVS to reduce PI in PD probably depends more on morphometric features of the brainstem which contains functionally important centers involved in the control of both posture and gait. Due to its high sensitivity and specificity, the MPR can be considered as a prognostic marker of the GVS effectiveness in the PI treatment.
Table.
Figure. ROC Analysis Results
To cite this abstract in AMA style:
O. Alenikova, A. Chumak A, G. Zobnina, D. Antonenka. MRI Predictive Marker of the Vestibular Galvanic Stimulation Effectiveness in the Postural Instability Treatment in Parkinson’s Disease. [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/mri-predictive-marker-of-the-vestibular-galvanic-stimulation-effectiveness-in-the-postural-instability-treatment-in-parkinsons-disease/. Accessed December 27, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/mri-predictive-marker-of-the-vestibular-galvanic-stimulation-effectiveness-in-the-postural-instability-treatment-in-parkinsons-disease/