Category: Other
Objective: Objective: This study aims to systematically review the array of movement disorders observed in patients diagnosed with brain sagging syndrome (BSS) secondary to spontaneous intracranial hypotension (SIH).
Background: Background: While BSS typically presents with chronic orthostatic headaches and behavioral/cognitive changes, a subset of patients may manifest with various involuntary movements. The underlying pathophysiology likely involves venous engorgement of deep brain structures and the brainstem, direct mechanical stress on subcortical structures, and tonsillar ectopy. As this condition is treatable, familiarity among neurologists with BSS and its associated involuntary movements is imperative.
Method: Methods: We performed a comprehensive literature search in PubMed in March 2024 using the Boolean phrase- ((“Brain sagging”) OR (“Intracranial hypotension”)) AND ((((((((((“Movement disorders”) OR (“Involuntary movements”)) OR (“Tremor”)) OR (“Dystonia”)) OR (“Chorea”)) OR (“Ballismus”)) OR (“Myorhythmia”)) OR (“Tic”)) OR (“Ataxia”)) OR (“Parkinsonism”)), which yielded 35 articles. Additional articles were identified by scrutinizing the references of all included articles.
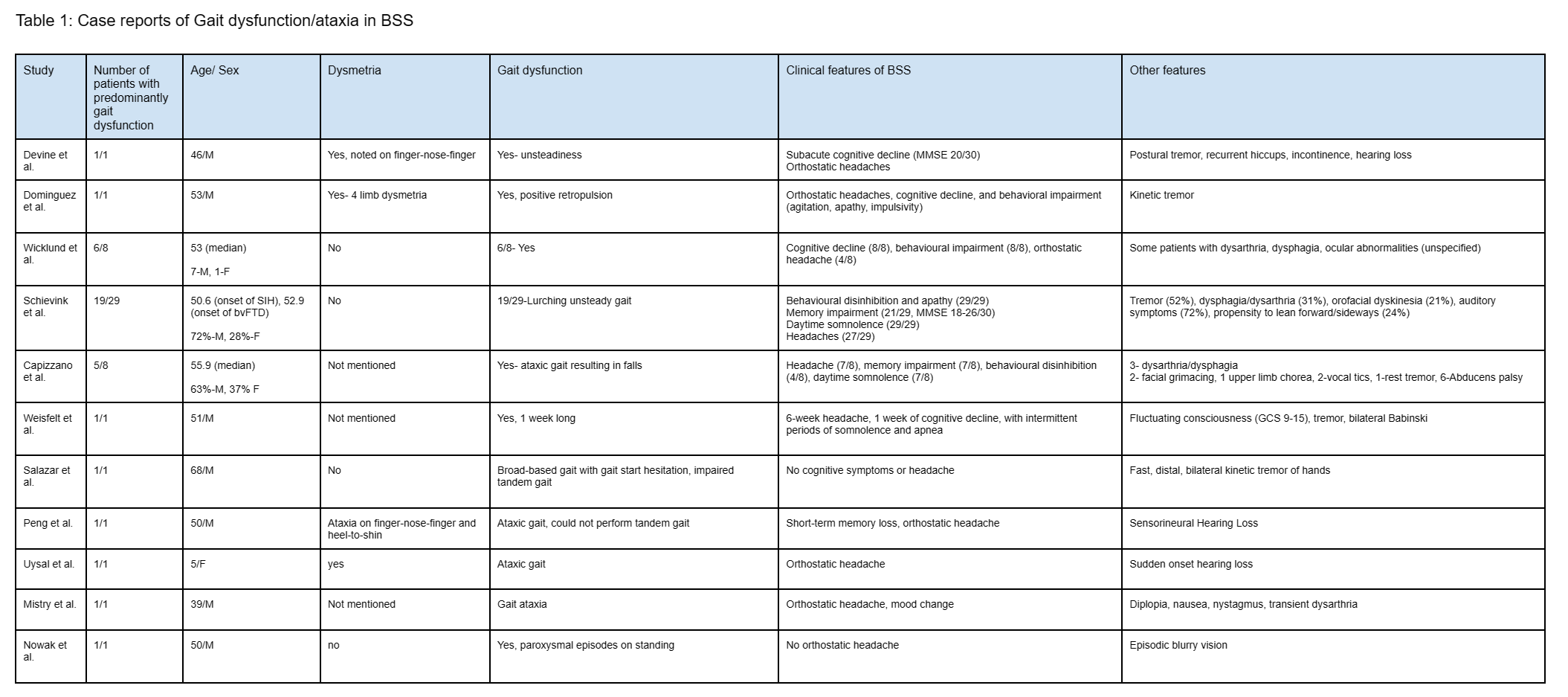
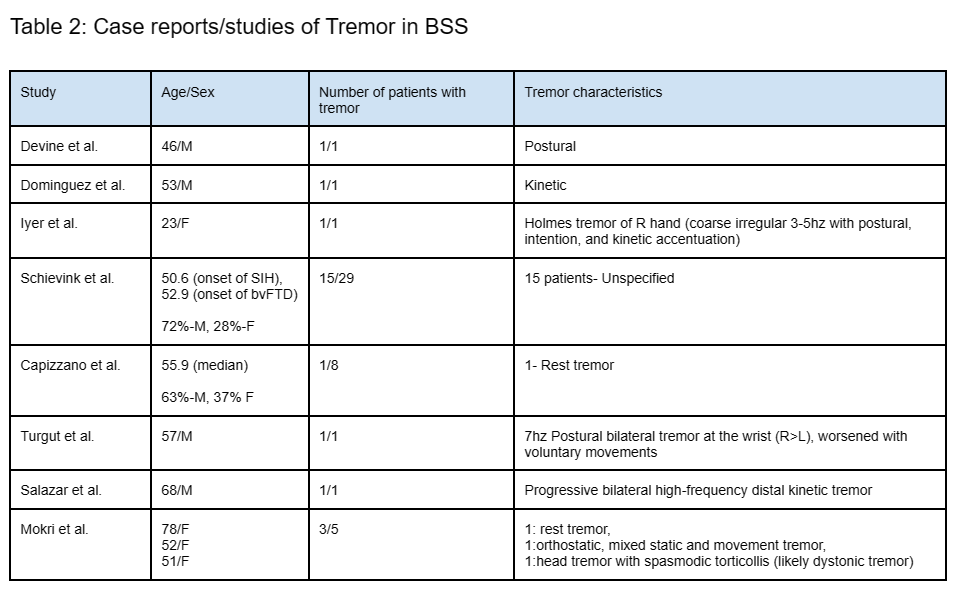
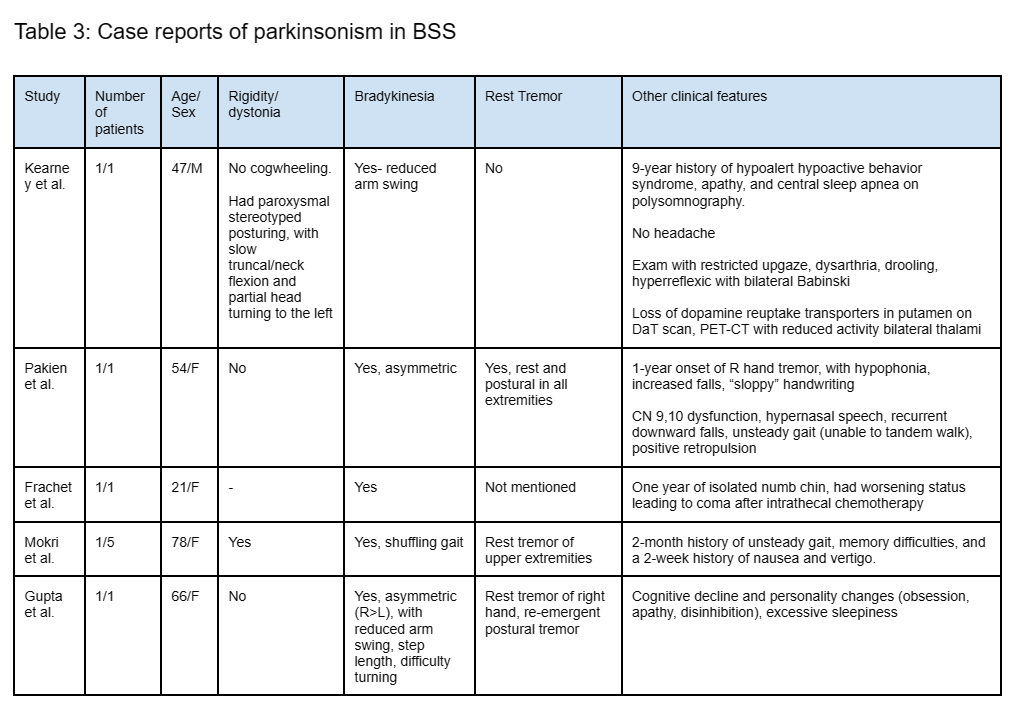
Results: Results: 18 articles reported movement disorders in the context of BSS, which classically occurs most often in males in their 50s [Tables 1,2,3]. Subacute gait ataxia was the most frequently reported movement disorder and this co-existed with the classic features of BSS, along with other signs suggestive of cerebellar involvement. The latter include ataxic dysarthria, nystagmus, dysmetria, and action tremor. However, rarely, gait ataxia can be the sole manifestation of BSS, can be episodic, and can be acute in onset. Tremor is frequently postural and kinetic (and rarely may be the first symptom). Parkinsonism, chorea, and dystonia (especially orofacial dyskinesias) can occur, and these may be associated with brainstem symptoms. One study noted compulsive repetitive truncal flexion associated with breath-holding in 35.3% of patients. MRI brain, in addition to signs of SIH, usually reveals a sagging/engorged brainstem, tonsillar ectopy, and venous engorgement; a leak may not always be found.
Conclusion: Conclusions: Given that it is eminently treatable with blood patches, subacute onset of movement disorders in the context of chronic headache or memory disturbance, should prompt inclusion of BSS as a differential diagnosis.
Table 1: Gait dysfunction/ataxia in BSS
Table 2: Tremor in BSS
Table 3: Parkinsonism in BSS
To cite this abstract in AMA style:
A. Datta, A. Lenka. Movement disorders in Brain Sagging Syndrome- A Systematic Review [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/movement-disorders-in-brain-sagging-syndrome-a-systematic-review/. Accessed December 12, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/movement-disorders-in-brain-sagging-syndrome-a-systematic-review/