Session Information
Date: Monday, September 23, 2019
Session Title: Other
Session Time: 1:45pm-3:15pm
Location: Agora 2 West, Level 2
Objective: We aim to highlight the spectrum of movement disorders in patients of autoimmune encephalitis (AE) diagnosed at our tertiary care center and describe their clinical symptoms, diagnostic approach, treatment and outcome.
Background: Autoimmune encephalitis constitutes an important treatable cause of movement disorders.1Increasing awareness and ease of antibody testing has led to a rise in number of patients being diagnosed with AE. However, the diversity of clinical presentation still serves as a barrier for the early diagnosis and treatment of the patients.2
Method: We evaluated nine patients who presented with movement disorders in association with AE at our tertiary care center. All patients were treated as per the standard protocol.1
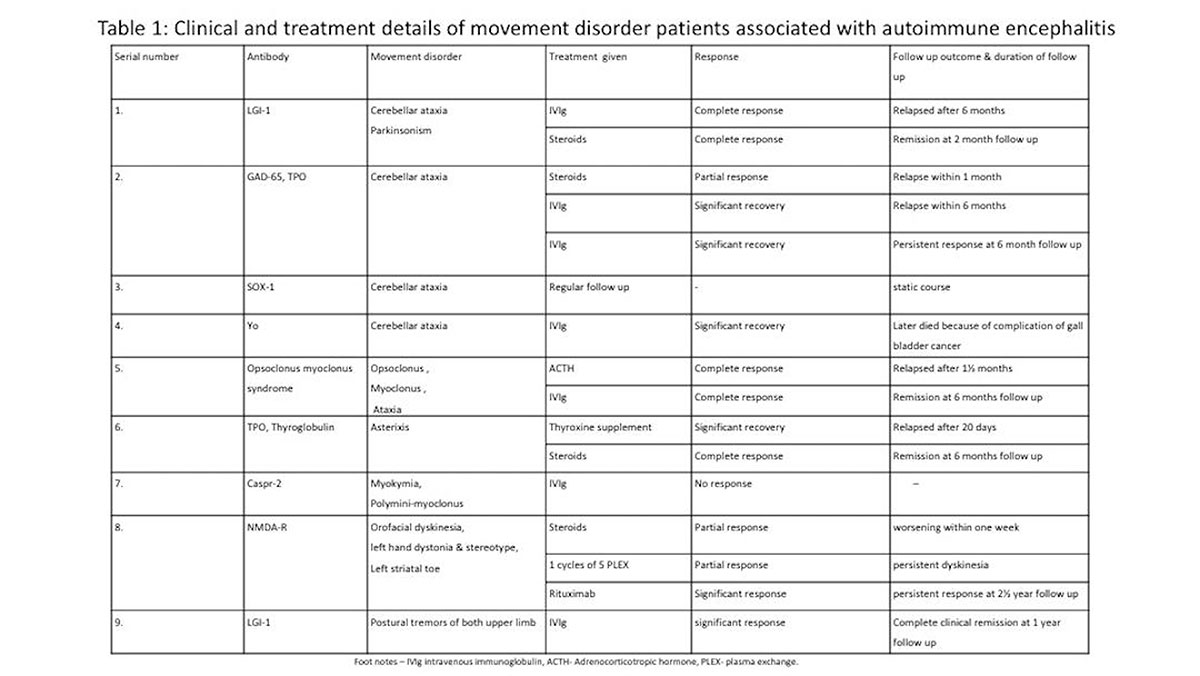
Results: There were 9 patients of AE who presented with movement disorders. Different movement disorders were observed in these patients, most common being cerebellar ataxia, which was present in 4 patients. These patients had antibodies against GAD-65, Yo, LGI-1 and opsoclonus myoclonus syndrome (OMS). Other movements observed included asterixis in Hashimoto’s encephalitis patient, polyminimyoclonus and myokymia in patient with anti-CASPR 2, orofacial dyskinesia,left hand dystonia, stereotypy and left striatal toe in NMDAR encephalitis patient and parkinsonism with postural tremors of hands in patients with anti-LGI 1 (Table 1). Out of the 9 patients, 5 had single type of movement disorder while rest 4 had more than one type of movement disorders. Among these nine patients, antibodies were detected against LGI-1 in 2 patients, GAD, CASPR- 2, SOX-1, Yo, NMDAR and TPO/TG each in one patient. One patient was diagnosed with OMS associated with neuroblastic tumour. Fivepatients responded well to single first-line immunotherapy (IVIg or steroid) while one responded partially to single first line therapy. One patient with NMDAR antibodies did not respond to steroids and PLEX. Then she received second line therapy consisting of rituximab. Relapse occurred in 3 of our patients.
Conclusion: Movement disorder is one of the most consistent feature of AE. Understanding of the ever-expanding spectrum of antibodies associated with movement disorders helps in the better management of such patients as reflected by the substantial proportion of patients diagnosed with AE associated movement disorders and successfully treated at our institution.
References: 1. Dash, D., and Pandey, S., Movement disorders associated with neuronal antibodies. Acta Neurologica Scandinavica. 2019;139:106 –117 2. Graus, F., Titulaer, M. J., Balu, R., Benseler, S., Bien, C. G., Cellucci et al. A clinical approach to diagnosis of autoimmune encephalitis. The Lancet Neurology. 2016;15(4):391– 404.
To cite this abstract in AMA style:
A. Chouksey, S. Pandey. Movement disorders associated with autoimmune encephalitis [abstract]. Mov Disord. 2019; 34 (suppl 2). https://www.mdsabstracts.org/abstract/movement-disorders-associated-with-autoimmune-encephalitis/. Accessed April 21, 2025.« Back to 2019 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/movement-disorders-associated-with-autoimmune-encephalitis/