Category: Parkinson's Disease: Cognitive functions
Objective: We explored potential bias to diagnose cognitive impairment in People with Parkinson’s (PwP) followed in the Parkinson’s Progressive Markers Initiative (PPMI).
Background: In primary care settings dementia diagnoses are often based on clinical impressions and reports from patients or others[1]. Without formal evaluation, other disorders such as depression can result in misdiagnosis[2]. The risk of misdiagnosis of Mild Cognitive Impairment (MCI) or dementia may be even higher in PwP, where motor and non-motor symptoms may bias impression of impairment.
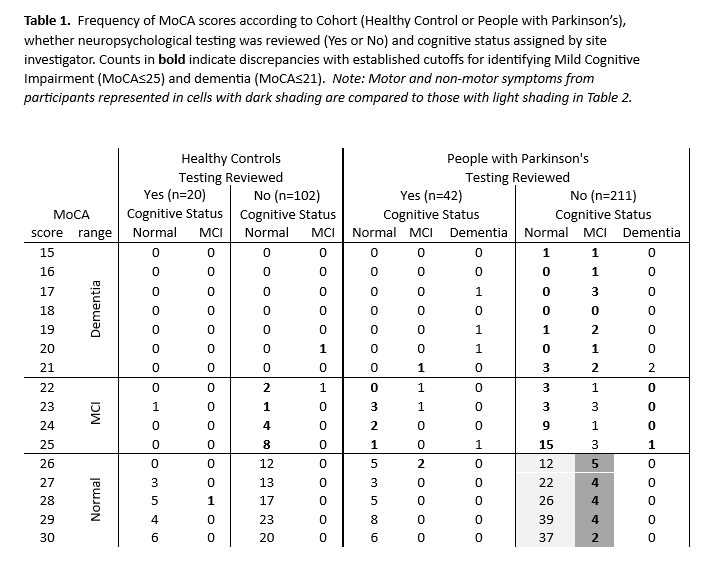
Method: A sample of 253 newly diagnosed PwP and 122 Health Controls (HC) completed baseline and 5-year follow-up assessments of motor, psychiatric, and cognitive functioning through the PPMI study. The cognitive battery included a screening measure, Montreal Cognitive Assessment (MoCA), and standardized tests of memory, language, visuospatial, and executive functions. Determination of cognitive impairment was made by the site principal investigator at the 5-year visit. Case record forms documented whether cognitive test results were reviewed when determining cognitive status. We identified possible cognitive misdiagnosis when MCI or dementia status was given to participants who performed above an established cutoff on the MoCA (≥26).[3]
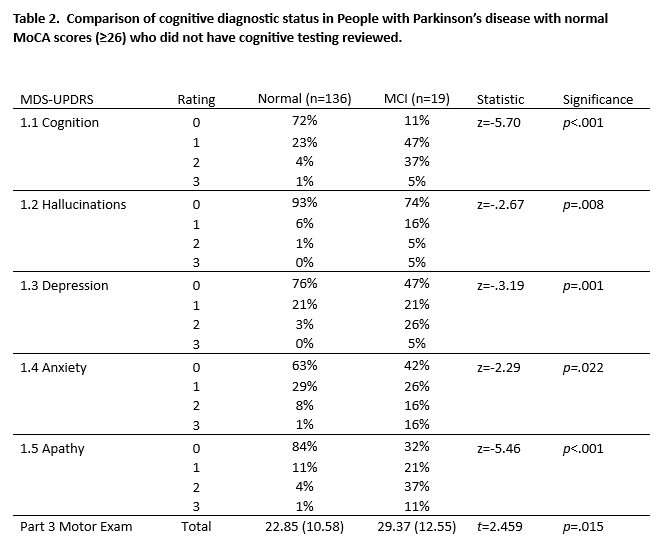
Results: Results from cognitive testing were infrequently used to determine cognitive status, HC=20 (16%), PwP=42 (17%). In HC, 15% of those considered normal performed below MoCA cutoff. [Table 1] In PwP, cognitive status closely matched MoCA cutoffs when cognitive testing was reviewed; however, MoCA scores were markedly discrepant when testing was not considered. \When testing was not reviewed, possible misdiagnosis of cognitive impairment in PwP with normal MoCA scores (n=19, dark shaded cells in Table 1) was associated with elevated non-motor symptom ratings from Part 1 of the MDS-UPDRS, and higher overall motor dysfunction on Part 3 [Table 2].
Conclusion: Our results suggest that cognitive testing is not often considered when diagnosing cognitive impairment in PwP. In the absence of test results, psychiatric symptoms and motor impairment may lead to overdiagnosis of cognitive impairment, even among experts. These findings underscore the importance of formal testing as outlined in Movement Disorder Society Task Force consensus criteria for MCI [4] and dementia [5].
Table 1
Table 2
References: 1. Bradford A, Kunik ME, Schulz P, Williams SP, Singh H. Missed and delayed diagnosis of dementia in primary care: prevalence and contributing factors. Alzheimer Dis Assoc Disord. 2009;23(4):306-314.
2. Salem LC, Andersen BB, Nielsen TR, et al. Overdiagnosis of dementia in young patients – a nationwide register-based study. Dement Geriatr Cogn Disord. 2012;34(5-6):292-299.
3. Dalrymple-Alford JC, MacAskill MR, Nakas CT, et al. The MoCA: well-suited screen for cognitive impairment in Parkinson disease. Neurology. 2010;75(19):1717-1725.
4. Litvan I, Goldman JG, Troster AI, et al. Diagnostic criteria for mild cognitive impairment in Parkinson’s disease: Movement Disorder Society Task Force guidelines. Mov Disord. 2012;27(3):349–356.
5. Emre M, Aarsland D, Brown R, et al. Clinical diagnostic criteria for dementia associated with Parkinson’s disease. Mov Disord. 2007;22(12):1689-1837.
To cite this abstract in AMA style:
F. Rodriguez-Porcel, T. Turner. Misdiagnosis of Cognitive Impairment in Parkinson’s disease [abstract]. Mov Disord. 2024; 39 (suppl 1). https://www.mdsabstracts.org/abstract/misdiagnosis-of-cognitive-impairment-in-parkinsons-disease/. Accessed December 29, 2025.« Back to 2024 International Congress
MDS Abstracts - https://www.mdsabstracts.org/abstract/misdiagnosis-of-cognitive-impairment-in-parkinsons-disease/