Category: Drug-Induced Movement Disorders
Objective: To investigate the cause of chronic neuroleptic drug-induced parkinsonism (NIP) through examination of the profile of striatal monoaminergic nerve terminal density using positron emission tomography (PET) in comparison with Parkinson’s disease (PD).
Background: NIP is a heterogenenous and common cause of parkinsonism. Based on abnormal dopamine transporter (DAT)-scan results, individuals displaying irreversible NIP following drug withdrawal are diagnosed with PD, but this assumption needs further support. The vesicular monoamine transporter type 2 (VMAT2) protein has been proposed as a potentially less regulated PET target alternative to the DAT protein to label striatal monoaminergic terminals.
Method: Subjects between age 50-80 living with schizophrenia spectrum disorders under long-term stable antipsychotic drug treatment, with (N=11) or without (N=11) NIP, healthy volunteers (N=11), and patients medicated for Hoehn-Yahr stage 1-2 PD (N=12), were included. UPDRS-III motor ratings and olfactory data with the Brief 12-item Smell Identification Test (B-SIT, Sensonics) were collected, in addition to PET imaging acquisition with [11C](+)-dihydrotetrabenazine. Striatal dopamine D2 receptors availability drawn from [11C]raclopride binding potential was also examined. The performance of olfactory loss to detect participants with striatal presynaptic terminal defect on imaging was evaluated by receiver operating characteristic analysis.
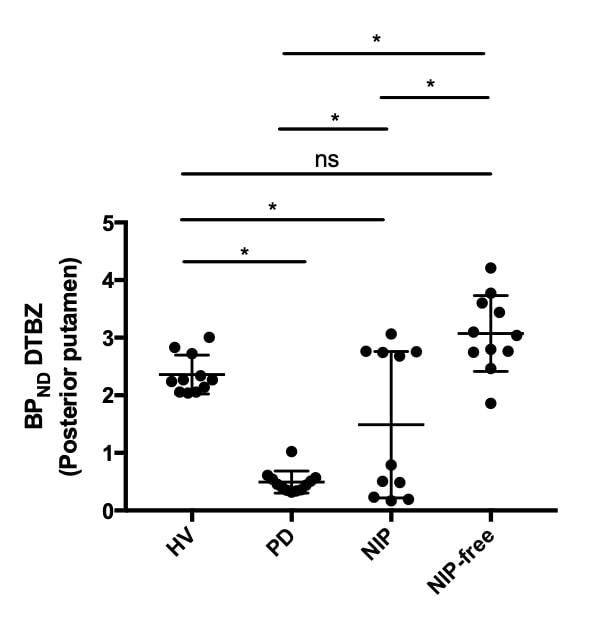
Results: Striatal VMAT2 binding potential was dichotomous in the NIP group between those with spared (N=5) or low (N=6) PD-like values [figure1]. Striatal binding reduction in the low VMAT2- subgroup was asymmetric and within PD range, but lacked the gradient of maximal involvement in the posterior putamen typical of PD. All but 4 patients under antipsychotic drug treatment displayed a reduction in putamen D2 receptors availability >60%, regardless of the motor phenotype. B-SIT percentile values in the range of anosmia were correlated with abnormal striatal VMAT2 binding status (AUC 0.894, p<0.0001).
Conclusion: These preliminary observations suggest that striatal VMAT2 binding is abnormal in a fraction of chronic NIP cases and differs in spatial distribution from PD. The possibility of a drug-induced axonopathy and resultant synaptopathy, as well as the evolution of the binding deficit, warrant further studies in a large cohort.
To cite this abstract in AMA style:
M. Galoppin, P. Berroir, J. Soucy, E. Stip, P. Blanchet. Mechanisms of chronic neuroleptic-induced parkinsonism examined with positron emission tomography [abstract]. Mov Disord. 2020; 35 (suppl 1). https://www.mdsabstracts.org/abstract/mechanisms-of-chronic-neuroleptic-induced-parkinsonism-examined-with-positron-emission-tomography/. Accessed April 25, 2025.« Back to MDS Virtual Congress 2020
MDS Abstracts - https://www.mdsabstracts.org/abstract/mechanisms-of-chronic-neuroleptic-induced-parkinsonism-examined-with-positron-emission-tomography/